- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- E/M Coding and Billing Res...
- Office/Outpatient E/M Visi...

Office/Outpatient E/M Codes
2021 e/m office/outpatient visit cpt codes.
The tables below highlight the changes to the office/outpatient E/M code descriptors effective in 2021.
More details about these office/outpatient E/M changes can be found at CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes.
All specific references to CPT codes and descriptions are © 2023 American Medical Association. All rights reserved. CPT and CodeManager are registered trademarks of the American Medical Association.
Download the Office E/M Coding Changes Guide (PDF)

Preventative Medicine vs. Evaluation and Management Codes
- By Terry A. Fletcher BS, CPC, CCC, CEMC, CCS, CCS-P, CMC, CMSCS, ACS-CA, SCP-CA, QMGC, QMCRC, QMPM
- July 18, 2020

Choosing a proper office visit code can become confusing unless one understands the rules separating preventative medicine and evaluation and management coding.
Preventative medicine codes are meant only for the reporting of asymptomatic patients. In order to assign a preventative code, a comprehensive evaluation must be documented. The scope of a preventative visit depends both on the patient’s age and screening test(s) fitting the age of the patient.
Medicare does not cover the CPT codes 99381-99397 (preventative medicine services). When billing a preventative medicine visit for a Medicare patient, a waiver of liability is NOT required. This is based on the Social Security Act, Section 1862(a)(7), Statutory Exclusion. The patient is responsible for 100% of the accumulated debt in such instances. The amount that other commercial insurance carriers will pay depends on whether these services are included in the individual’s insurance plan.
Coding Guidelines for CPT Preventive Medicine Services
In CPT, codes 99381–99397 for comprehensive preventive evaluations are age-specific, beginning with infancy and ranging through patients age 65 and over for both new and established office patients. Preventive medicine services are represented in evaluation and management (E/M) codes section of CPT. These E/M codes may be reported by any qualified physician or other qualified healthcare professional, i.e. NP, APP or PA.
Components of a Preventive Medicine Visit:
Preventive visits, like many procedural services, are bundled services. Unlike documenting problem-oriented E/M office visits (99201–99215), which involves complicated coding guidelines, documenting preventive visits is more straightforward. The following components are needed:
- A comprehensive history and physical exam findings;
- A description of the status of chronic, stable problems that are not “significant enough to require additional work,” according to CPT;
- Notes concerning the management of minor problems that do not require additional work;
- Notes concerning age-appropriate counseling, screening labs, and tests;
- Orders for vaccines appropriate for age and risk factors.
According to CPT, the comprehensive history that must be obtained as part of a preventive visit has no chief complaint or present illness as its focus. Rather, it requires a “comprehensive system review and comprehensive or interval past, family, and social history as well as a comprehensive assessment/history of pertinent risk factors.” The preventive comprehensive exam differs from a problem-oriented comprehensive exam because its components are based on age and risk factors rather than a presenting problem.
Coverage of preventive visits varies by insurer, so it is important to be aware of the patient’s health plan. Most plans limit the frequency of the preventive visit to once a year, and not all tests are covered. Fecal occult blood tests, audiometry, Pap smear collection, and vaccines and their administration should be billed separately. Visual acuity testing is not separately reimbursed.
Without a new or chronic-disease diagnosis, all labs and other tests ordered during a preventive visit are for screening purposes, and an ICD-10-CM code for screening should be assigned on the order form and claim.
When billing for a preventative medicine visit, it is legal to also bill for an evaluation and management service if a patient wants a medical problem addressed at the time of their yearly physical exam. What you have to be careful of is a patient who presents with well-controlled chronic conditions with no complaints and is there to “establish care”. That may be considered a preventative visit to Medicare and Commercial plans.
The following is an example of when to consider billing a separate Evaluation and Management visit code in addition to a Preventative Medicine visit service:
An internal medicine physician sees an established patient Medicare aged patient for their scheduled yearly exam (preventative medicine). The patient did not mention any complaints when the appointment was made and stated that he wanted to be seen for an annual physical only. However, during the course of the visit, the physician determines that the patient has an enlarged prostate. This finding requires an evaluation and work-up that is separate from a preventative history and physical service.
If the internist finds a problem while performing an annual physical, and if the problem is “significant enough” to warrant additional testing, prescribing, or problem-work up, then the appropriate office visit code 99212-99215 should also be reported with a 25 modifier, to reflect the “significant separately identifiable service”. The services should be coded as 99397 (preventative established patient over 65 years old) and 99212-99215-25 for the evaluation and discussion of the enlarged prostate, depending on the documentation level of the E/M visit.
Plenty of practice managers have been faced with the question of whether to bill for a preventative medicine visit or an E&M level of service. The answer is relatively simple, bill according to the “intent” of the visit. If the objective is to provide an annual asymptomatic physical, then a preventative medicine code should be reported. Some sources state that you may bill a preventative medicine visit with a chronic condition such as hypertension or diabetes. If a physician is only managing a patient’s medication, there are no changes or concerns, and the patient then it would be appropriate to bill for preventative medicine. However, if a physician needs to make changes to that medication after finding out that it is causing side effects, utilize a proper evaluation and management visit code.
This is controversial, as the guidelines for the preventative services, in CPT references a subsection that states, “If an abnormality is encountered or a pre-existing problem is addressed in the process of performing this preventive medicine E/M service, and if the problem or abnormality is significant enough to require additional work to perform the key components of a problem-oriented E/M service, then the appropriate Office/Outpatient code 99201-99215 should also be reported.”
CPT goes on to say:
“An insignificant or trivial problem/abnormality that is encountered in the process of performing the preventive medicine E/M and which does not require additional work and the performance of the key components of a problem-oriented E/M service should not be reported.”
Only the physician can determine if the abnormality is “significant” enough to warrant two E/M services, and many times, there is a double co-pay for commercial plans and a higher out of pocket for Medicare patients. It may be a better idea to pick either a problem-oriented E/M visit over the preventative medicine visit and save that for another day. Again, it is a physician’s judgement, based on the level of care that was administered that day.
I would not want to see the decision based on the patient’s potential out of pocket share of cost, but it is a factor, when you consider what the patient scheduled. You’ll find most patients expect a “free” visit when they schedule a “yearly exam”. It’s important to explain to the patient that two separate services are being performed so they may expect additional charges, but it saves them the inconvenience of a second visit to address them both now.
CPT Assistant weighed in on this topic in 2009, and gave 2 examples of a preventative visit, again that was age and gender appropriate:
- Preventative Service for a 33-year-old woman, may include a pap and pelvic, breast exam and BP check. Counseling may be diet, exercise, substance abuse and sexual activity.
- For a 13-year old girl, it may include a scoliosis screen, assessment of growth, development, behavior, immunizations. Anticipatory guidance, health habits, self-care, avoidance of substances, avoiding risks associated with sexual activity, and even wearing a seatbelt while in a care.
But when would it be appropriate here to bill for an office visit in addition to the preventative service?
Take example 1. During the female adult preventative exam, the physician identifies a palpable solitary lump in her right breast. The physician finds this “significant” enough to require additional work, and to perform the key components of a problem-oriented E/M service. So 99395 would be reported for the preventative visit, and 99213-25 would be reported for the visit related to the breast lump.
Now in saying this, there are “covered services” under the umbrella of “preventative” that do not include an actual comprehensive exam or comprehensive history, but more of a “review” or current inventory of the overall health of the patient. The IPPE (see chart below) has minimal exam elements to include:
- Height, weight, body mass index, and blood pressure ● Visual acuity screen ● Other factors deemed appropriate based on the beneficiary’s medical and social history and current clinical standards
Also, know the difference in what you are reporting. For Medicare beneficiaries there are 3 options:
Source: CMS MLN Booklet ICN 006904 August 2018
For additional guidelines regarding preventative medicine and evaluation and management coding, please refer to the American Medical Association (AMA) or Centers for Medicare & Medicaid Services (CMS) website.
Other References:
http://img.medscape.com/article/748/528/Comparing.pdf
https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/mps_qri_ippe001a.pdf
- TAGS: CPT , E&M

Terry A. Fletcher BS, CPC, CCC, CEMC, CCS, CCS-P, CMC, CMSCS, ACS-CA, SCP-CA, QMGC, QMCRC, QMPM
Related stories.

Modifier 25: Where, When, and How to Use It Correctly
Modifier 25 remains that prickly modifier that seems to be a part of strategic planning for payment reduction to providers by health plans. For anyone

The Front Line of Climate Change: How Healthcare Coders Are Making a Difference
Climate change is no longer a distant threat; it’s a current reality affecting all facets of life, including public health. As the planet warms, healthcare
Leave a Reply
Please log in to your account to comment on this article.
Featured Webcasts

Comprehensive Outpatient Clinical Documentation Integrity: From Foundations to Advanced Strategies
Optimize your outpatient clinical documentation and gain comprehensive knowledge from foundational practices to advanced technologies, ensuring improved patient care and organizational and financial success. This webcast bundle provides a holistic approach to outpatient CDI, empowering you to implement best practices from the ground up and leverage advanced strategies for superior results. You will gain actionable insights to improve documentation quality, patient care, compliance, and financial outcomes.

Advanced Outpatient Clinical Documentation Integrity: Mastering Complex Narratives and Compliance
Enhancing outpatient clinical documentation is crucial for maintaining accuracy, compliance, and proper reimbursement in today’s complex healthcare environment. This webcast, presented by industry expert Angela Comfort, DBA, RHIA, CDIP, CCS, CCS-P, will provide you with actionable strategies to tackle complex challenges in outpatient documentation. You’ll learn how to craft detailed clinical narratives, utilize advanced EHR features, and implement accurate risk adjustment and HCC coding. The session also covers essential regulatory updates to keep your documentation practices compliant. Join us to gain the tools you need to improve documentation quality, support better patient care, and ensure financial integrity.

Foundations of Outpatient Clinical Documentation Integrity: Best Practices for Accurate Coding and Compliance
This webcast, presented by Angela Comfort, DBA, RHIA, CDIP, CCS, CCS-P, a recognized expert with over 30 years of experience, offers essential strategies to improve outpatient clinical documentation integrity. You will learn how to enhance the accuracy and completeness of patient records by adopting best practices in coding and incorporating Social Determinants of Health (SDOH). The session also highlights the role of technology, such as EHRs and CDI software, in improving documentation quality. By attending, you will gain practical insights into ensuring precise and compliant documentation, supporting patient care, and optimizing reimbursement. This webcast is crucial for those looking to address documentation gaps and elevate their coding practices.

Preventing Sepsis Denials: From Recognition to Clinical Validation
ICD10monitor has teamed up with renowned CDI expert Dr. Erica Remer to bring you an exclusive webcast on how to recognize sepsis, how to get providers to give documentation that will support sepsis, and how to educate to avert sepsis denials. Register now and become a crucial piece of the solution to standardizing sepsis clinical practice, documentation, and coding at your facility.
Trending News

A Two-Year Anniversary

National Study: Artificial Intelligence Helps Patients When Refilling Prescriptions


National Progress Reported in Reducing Medical Errors: Leapfrog Group CEO to Report Findings on Talk Ten Tuesdays

DOJ Launches New Whistleblower Award Program Aimed at Attracting Tips about Healthcare Fraud

Pediatric SDoH: An Essential Guide to Accurate Coding and Reporting
This webcast, presented by Tiffany Ferguson, LMSW, CMAC, ACM, addresses the critical gap in Social Determinants of Health (SDoH) reporting for pediatric populations. While SDoH efforts often focus on adults, this session emphasizes the unique needs of children. Attendees will gain insights into the current state of SDoH, new pediatric Z-codes, and the importance of interdisciplinary collaboration. By understanding and applying pediatric-specific SDoH factors, healthcare professionals can improve data capture, compliance, and care outcomes. This webcast is essential for those looking to enhance their approach to pediatric SDoH reporting and coding.

Oncology and E/M Services: Compliance, Medical Necessity, and Reimbursement
Join Becky Jacobsen, BSN, RN, MBS, CCS-P, CPC, CPEDC, CBCS, CEMC, VP of CDM, for a webcast addressing oncology service coding challenges. Learn to navigate coding for infusions and injections alongside Evaluation and Management (E/M) services, ensuring compliance and accurate reimbursement. Gain insights into documenting E/M services for oncology patients and determining medical necessity. This webcast is essential to optimize coding practices, maintain compliance, and maximize revenue in oncology care.

The Inpatient Admission Order: Master the Who, When, and How
During this webcast Dr. Ronald Hirsch delves into the inpatient admission order process including when to get it, when it becomes effective, its impact on billing and payment, who can write it, how to cancel it, the effects on the beneficiary, and more. You’ll leave with a clear understanding of inpatient orders and guidelines for handling improper orders that you can implement immediately.

Navigating AI in Healthcare Revenue Cycle: Maximizing Efficiency, Minimizing Risks
Michelle Wieczorek explores challenges, strategies, and best practices to AI implementation and ongoing monitoring in the middle revenue cycle through real-world use cases. She addresses critical issues such as the validation of AI algorithms, the importance of human validation in machine learning, and the delineation of responsibilities between buyers and vendors.

Leveraging Generative and Advanced AI to Transform Coding and CDI – Part 1

Job Cuts – When They Impacts You

Coding Reviews Can Be Complex

Understanding Business Intelligence and the Impact of AI
Stay connected.
Subscribe to receive free ICD-10 news and updates.
5874 Blackshire Path, #13 Inver Grove Heights, MN 55076
Hours: 9am – 5pm CT Phone: (800) 252-1578 Email: [email protected]
Copyright © 2024 ICD10monitor. Powered by MedLearn Media.

Prepare for the 2025 CMS IPPS Final Rule with ICD10monitor’s IPPSPalooza! Click HERE to learn more
Get 15% OFF on all educational webcasts at ICD10monitor with code JULYFOURTH24 until July 4, 2024—start learning today!
Advanced Search Help
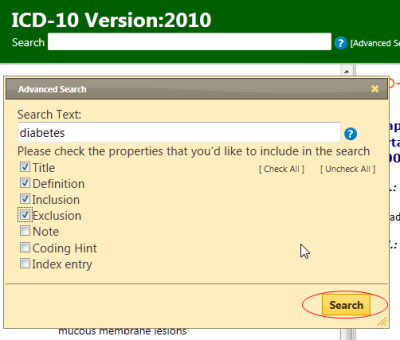
Advanced search lets you search selected properties of the classification. You could search all properties or a selected subset only
First, you need to provide keywords in the Search Text field then check the properties that you'd like to include in the search.
The system will search for the keywords in the properties that you've checked and rank the results similar to a search engine
The results will be displayed in the Search Results pane. If the search query hits more than 200 results, then only the top 200 will be displayed.
If you provide more than one keyword, the system will search for items that have all the keywords.
Wildcards: You may also use wildcard character * . see examples below.
OR operator : It's possible to have the results that have either one or another keyword. Please see the example 4.
1. Search Text: diabetes {finds all that have the word "diabetes" in the searched fields}
2. Search Text: diabet* {finds all that have a word that start with "diabet" }
3. Search Text: diabet* mellitus {finds all that have a word that starts with "diabet" and also contains the word "mellitus"}
4. Search Text: tubercul* (lung OR larynx) { finds all that have a word that starts with "tubercul" and than has either lung OR larynx in it
Search Results
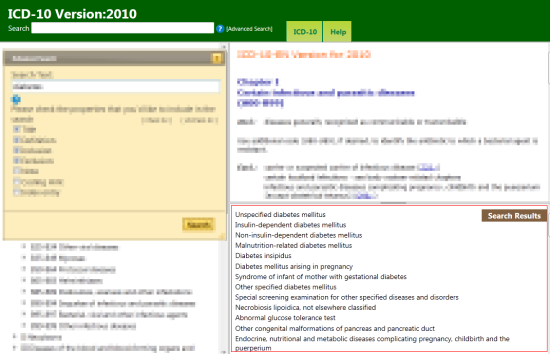
After the search the results are displayed at the lower right area of the screen. Here the porgram lists the titles of the ICD categories in which your search keywords are found.
Clicking on any result will take you to that category
You may close the advanced search window by clicking the X at the top left corner of the window.
The search results pane can be resized by dragging the horizontal line above it
ICD-10 Version:2016
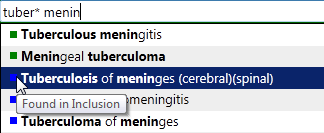
Quick search help.
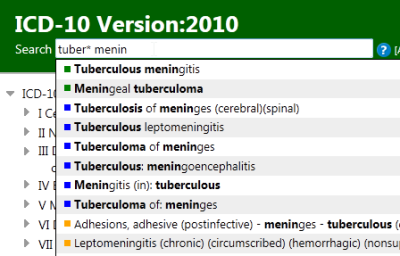
Quick search helps you quickly navigate to a particular category. It searches only titles, inclusions and the index and it works by starting to search as you type and provide you options in a dynamic dropdown list.
You may use this feature by simply typing the keywords that you're looking for and clicking on one of the items that appear in the dropdown list. The system will automatically load the item that you've picked.
You may use wildcards '*' as well to find similar words or to simply save some typing.
For example, tuber* confirmed will hit both tuberculosis and tuberculous together with the word 'confirmed'
If you need to search other fields than the title, inclusion and the index then you may use the advanced search feature
You may also use ICD codes here in order to navigate to a known ICD category.
The colored squares show from where the results are found. ( green:Title, blue:inclusions, orange:index, red:ICD code) You don't need to remeber the colors as you may hover your mouse on these squares to read the source.
- ICD-10 Version:2019 - English
- ICD-10 Version:2015 - English
- ICD-10 Version:2014 - English
- ICD-10 Version:2010 - English
- ICD-10 Version:2008 - English
- ICD-10 Version:2008 - French
- Older versions
- ICD-10 Instruction Manual
- List of Changes
- ICD Home Page
- ICD-10 Online Training

International Statistical Classification of Diseases and Related Health Problems 10th Revision
You may browse the classification by using the hierarchy on the left or by using the search functionality
More information on how to use the online browser is available in the Help


IMAGES
COMMENTS
Z02.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2024 edition of ICD-10-CM Z02.9 became effective on October 1, 2023. This is the American ICD-10-CM version of Z02.9 - other international versions of ICD-10 Z02.9 may differ. Z codes represent reasons for encounters. A ...
ICD-10-CM Code for Encounter for general adult medical examination without abnormal findings Z00.00 ICD-10 code Z00.00 for Encounter for general adult medical examination without abnormal findings is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
Learn how to code office visits using total time or medical decision making (MDM) without counting data points. Follow a four-step process to determine the level of service based on problems, data, and risk.
Z00.01 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Encounter for general adult medical exam w abnormal findings; The 2024 edition of ICD-10-CM Z00.01 became effective on October 1, 2023.
According to the 2024 ICD-10-CM Official Guidelines for Coding and Reporting, ... The Purpose of an Office Visit. Office visits focus on treatment to return the patient to wellness. These visits are designed to discuss new or existing health issues, concerns, worries, or symptoms. The provider may prescribe or change the patient's medication ...
Learn how to apply the new AMA guidelines for coding and documenting office visit/outpatient E/M services, effective Jan. 1, 2021. See examples of common visit types and how to select the level of service based on medical decision making or total time.
published on the NCHS website. The ICD-10-CM is a morbidity classification published by the United States for classifying diagnoses and reason for visits in all health care settings. The ICD-10-CM is based on the ICD-10, the statistical classification of disease published by the World Health Organization (WHO).
After the 2021 E/M office visit coding changes, most family physicians can find the right code for many of their visits just by answering these two questions. (Part One of a five-part series on E ...
The following ICD-10-CM Code Edits are applicable to this code: Adult diagnoses - The Medicare Code Editor detects inconsistencies in adult cases by checking a patient's age and any diagnosis on the patient's record. The adult code edits apply to patients age range is 15-124 years inclusive (e.g., senile delirium, mature cataract). ...
Z00.00 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Encntr for general adult medical exam w/o abnormal findings The 2024 edition of ICD-10-CM Z00.00 became effective on October 1, 2023.
Look to ICD-10-CM encounter codes when the testing is preventive, not diagnostic. ICD-10-CM diagnosis codes support medical necessity by identifying the. ... A screening Z code also may be used as an additional code if the screening is done during an office visit for other problems. A procedure code is required to confirm the screening was ...
October 1, 2017 Reporting Follow‐Up Encounters Q. How do I report an encounter for a follow‐up visit when the condition has been resolved? A. Per the ICD‐10‐CM guidelines "Do not code conditions that were previously treated and no longer exist." "The follow‐up codes (Z08, Z09, Z39) are used to explain continuing surveillance
Other insurers use CPT code 99417, which is for established patient visits of 55 minutes or more and new patient visits of 75 minutes or more. With both codes, prolonged services are billed in 15 ...
ICD 10 code for Person encountering health services to consult on behalf of another person. Get free rules, notes, crosswalks, synonyms, history for ICD-10 code Z71.0. ... Pre-adoption pediatrician visit for adoptive parent(s) Z76.81) The following code(s) above Z71.0 contain annotation back-references.
Learn about the changes to the office/outpatient E/M code descriptors effective in 2021. Compare the new and prior code descriptors for new and established patients based on history, examination, and medical decision making.
Choosing a proper office visit code can become confusing unless one understands the rules separating preventative medicine and evaluation and management coding. Preventative medicine codes are meant only for the reporting of asymptomatic patients. In order to assign a preventative code, a comprehensive evaluation must be documented. The scope of a preventative visit depends both […]
Quick Search Help. Quick search helps you quickly navigate to a particular category. It searches only titles, inclusions and the index and it works by starting to search as you type and provide you options in a dynamic dropdown list.. You may use this feature by simply typing the keywords that you're looking for and clicking on one of the items that appear in the dropdown list.
Care components. Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter.
Learn how to identify and code level 4 outpatient E/M visits based on total time or medical decision making under the 2021 rules. Find out the criteria, tips, and examples for each element of level 4 visits.
CPT® code 99213: Established patient office or other outpatient visit, 20-29 minutes. As the authority on the CPT® code set, the AMA is providing the top-searched codes to help remove obstacles and burdens that interfere with patient care. These codes, among the rest of the CPT code set, are clinically valid and updated on a regular basis to ...
Health care provider office as place; Physician office as the place of occurrence of the external cause. ICD-10-CM Diagnosis Code W94.11XD [convert to ICD-9-CM] Exposure to residence or prolonged visit at high altitude, subsequent encounter. Expsr to resdnce or prolonged visit at high altitude, subs.
40-54. All times in minutes. For longer visits there is a prolonged visit code, 99417, that should be reported with 99205/99215 for every 15 minutes that total time exceeds the ranges for those ...
Split (or Shared) E/M Services. CPT Codes 99202-99205, 99212-99215, 99221-99223, 99231-99239, 99281-99285, & 99291-99292. A split (or shared) service is an E/M visit where both a physician and NPP in the same group each personally perform part of a visit that each 1 could otherwise bill if provided by only 1 of them.