What is a mammogram?
A mammogram is an x-ray picture of the breast.
Mammograms can be used to check for breast cancer in women who have no signs or symptoms of the disease. This type of mammogram is called a screening mammogram. Screening mammograms usually involve two or more x-ray pictures, or images, of each breast. The x-ray images often make it possible to detect tumors that cannot be felt. Screening mammograms can also find microcalcifications (tiny deposits of calcium ) that sometimes indicate the presence of breast cancer.
Mammograms can also be used to check for breast cancer after a lump or other sign or symptom of the disease has been found. This type of mammogram is called a diagnostic mammogram. Besides a lump, signs of breast cancer can include breast pain, thickening of the skin of the breast, nipple discharge , or a change in breast size or shape; however, these signs may also be signs of benign conditions. A diagnostic mammogram can also be used to evaluate changes found during a screening mammogram or to view breast tissue when it is difficult to obtain a screening mammogram because of special circumstances, such as the presence of breast implants .

How are screening and diagnostic mammograms different?
The same machines are used for both types of mammograms. However, diagnostic mammography takes longer to perform than screening mammography and the total dose of radiation is higher because more x-ray images are needed to obtain views of the breast from several angles. The technologist may magnify a suspicious area to produce a detailed picture that can help the doctor make an accurate diagnosis.
What are the benefits and potential harms of screening mammograms?
Early detection of breast cancer with screening mammography means that treatment can be started earlier in the course of the disease, possibly before it has spread. Randomized clinical trials and other studies show that screening mammography can help reduce deaths from breast cancer among women ages 40 to 74 years at average risk of breast cancer, with the evidence of benefit being strongest for women ages 50 to 69 years ( 1 , 2 ). However, no studies to date have shown a benefit from regular screening mammography in women under age 40 or from baseline screening mammograms (mammograms used for comparison) taken before age 40.
The benefits of screening mammography need to be balanced against its harms, which include:
False-positive results. False-positive results occur when radiologists see an abnormality (that is, a potential “positive”) on a mammogram but no cancer is actually present. All abnormal mammograms should be followed up with additional testing (diagnostic mammograms, ultrasound , and/or biopsy ) to determine whether cancer is present.
False-positive mammogram results can lead to anxiety and other forms of psychological distress in affected women. The additional testing required to rule out cancer can also be costly and time consuming and can cause physical discomfort.
False-positive results are more common for younger women, women with dense breasts, women who have had previous breast biopsies, women with a family history of breast cancer, and women who are taking estrogen (for example, menopausal hormone therapy ). The chance of having a false-positive result increases with the number of mammograms a woman has. More than 50% of women screened annually for 10 years in the United States will experience a false-positive result, and many of these women will have a biopsy.
Overdiagnosis and overtreatment. Screening mammograms can find cancers and cases of ductal carcinoma in situ (DCIS, a noninvasive tumor in which abnormal cells that may become cancerous build up in the lining of breast ducts) that need to be treated. However, they can also find cases of DCIS and small cancers that would never cause symptoms or threaten a woman’s life. This phenomenon is called "overdiagnosis." Treatment of overdiagnosed cancers and overdiagnosed cases of DCIS is not needed and results in "overtreatment."
Because doctors cannot easily distinguish cancers and cases of DCIS that need to be treated from those that do not, they are all treated.
False-negative results. In cancer screening, a negative result means no abnormality is present. False-negative results occur when mammograms appear normal even though breast cancer is present. Overall, screening mammograms miss about 20% of breast cancers that are present at the time of screening. False-negative results can lead to delays in treatment and a false sense of security for affected women.
One cause of false-negative results is high breast density . Breasts contain both dense tissue (i.e., glandular tissue and connective tissue , together known as fibroglandular tissue) and fatty tissue. Fatty tissue appears dark on a mammogram, whereas fibroglandular tissue appears as white areas. Because fibroglandular tissue and tumors have similar density, tumors can be harder to detect in women with denser breasts.
False-negative results occur more often among younger women than among older women because younger women are more likely to have dense breasts. As a woman ages, her breasts usually become more fatty, and false-negative results become less likely.
Some breast cancers grow so quickly that they appear within months of a normal (negative) screening mammogram. This situation does not represent a false-negative result, because the negative result of the screening was correct. But it means that a negative result can give a false sense of security. Some of the cancers missed by screening mammograms can be detected by clinical breast exams (physical exams of the breast done by a health care provider).
Finding breast cancer early may not reduce a woman’s chance of dying from the disease. Even though mammograms can detect malignant tumors that cannot be felt, treating a small tumor does not always mean that the woman will not die from the cancer. A fast-growing or aggressive cancer may have already spread to other parts of the body before it is detected. Instead, women with such tumors live a longer period of time knowing that they likely have a potentially fatal disease.
In addition, finding breast cancer early may not help prolong the life of a woman who is suffering from other, more life-threatening health conditions.
Radiation exposure. Mammograms require very small doses of radiation. The risk of harm from this radiation exposure is low, but repeated x-rays have the potential to cause cancer. Although the potential benefits of mammography nearly always outweigh the potential harm from the radiation exposure, women should talk with their health care providers about the need for each x-ray. In addition, they should always let their health care provider and the x-ray technologist know if there is any possibility that they are pregnant, because radiation can harm a growing fetus.
Where can I find current recommendations for screening mammography?
Many organizations and professional societies, including the United States Preventive Services Task Force (which is convened by the Agency for Healthcare Research and Quality, a federal agency), have developed guidelines for mammography screening. All recommend that women talk with their doctor about the benefits and harms of mammography, when to start screening, and how often to be screened.
Although NCI does not issue guidelines for cancer screening, it conducts and facilitates basic, clinical, and translational research that informs standard clinical practice and medical decision making that other organizations may use to develop guidelines.
What is the best method of screening for breast cancer?
Regular high-quality screening mammograms and clinical breast exams are the most sensitive ways to screen for breast cancer.
Regular breast self-exam, or BSE—that is, checking one’s own breasts for lumps or other unusual changes—is not specifically recommended for breast cancer screening. In clinical trials, BSE alone was not found to help reduce the number of deaths from breast cancer.
However, many women choose to examine their own breasts. Women who do so should remember that breast changes can occur because of pregnancy, aging, or menopause ; during menstrual cycles; or when taking birth control pills or other hormones. It is normal for breasts to feel a little lumpy and uneven. Also, it is common for breasts to be swollen and tender right before or during a menstrual period. Whenever a woman notices any unusual changes in her breasts, she should contact her health care provider.
What is the Breast Imaging Reporting and Database System (BI-RADS®)?
The American College of Radiology (ACR) has established a uniform way for radiologists to describe mammogram findings. The system, called BI-RADS, includes seven standardized categories, or levels. Each BI-RADS category has a follow-up plan associated with it to help radiologists and other physicians appropriately manage a patient’s care.
Breast Imaging Reporting and Database System (BI-RADS)
BI-RADS also includes four categories of breast density that may be reported. The radiologist who reads the mammogram chooses the category that best describes the level of breast density seen on the mammogram film. The categories, from the least amount of breast density to the highest, are as follows:
- The breasts are almost entirely fatty
- There are scattered areas of dense glandular tissue and fibrous connective tissue (together known as fibroglandular density)
- The breasts are heterogeneously dense, which means they have more of these areas of fibroglandular density. This may make it hard to see small masses in the breast tissue on a mammogram.
- The breasts are extremely dense, which makes it hard to see tumors in the breast tissue on a mammogram.
Many states in the U.S. have enacted laws requiring mammography providers to tell women if they have dense breasts (i.e., breasts that are heterogeneously or extremely dense on a mammogram) and to inform them of risks associated with having dense breasts. In addition to making mammograms harder to read, dense breasts are a risk factor for breast cancer.
Where can women get high-quality mammograms?
Women can get high-quality mammograms in breast clinics, hospital radiology departments, mobile vans, private radiology offices, and doctors’ offices.
The Mammography Quality Standards Act (MQSA) is a federal law that requires mammography facilities across the nation to meet uniform quality standards. Under the law, all mammography facilities must: 1) be accredited by an FDA-approved accreditation body; 2) be certified by the FDA, or an agency of a state that has been approved by the FDA, as meeting the standards; 3) undergo an annual MQSA inspection; and 4) prominently display the certificate issued by the agency. More information about MQSA is available from the FDA .
Women can ask their doctors or staff at a local mammography facility about FDA certification before making an appointment. Women should look for the MQSA certificate at the mammography facility and check its expiration date. MQSA regulations also require that mammography facilities give patients an easy-to-read report of their mammogram results.
Information about local FDA-certified mammography facilities is available through NCI’s Cancer Information Service at 1–800–4–CANCER (1–800–422–6237). Also, a searchable list of these facilities can be found on the FDA website.
How much does a mammogram cost?
Insurance plans governed by the federal Affordable Care Act must cover screening mammography as a preventive benefit every 1–2 years for women age 40 and over without requiring copayments, coinsurance, or deductibles. In addition, many states require that Medicaid and public employee health plans cover screening mammography. Women should contact their mammography facility or health insurance company for confirmation of the cost and coverage.
Medicare pays for annual screening mammograms for all female Medicare beneficiaries who are age 40 or older. Medicare will also pay for one baseline mammogram for female beneficiaries between the ages of 35 and 39. There is no deductible requirement for this benefit. Information about coverage of mammograms is available on the Medicare website or through the Medicare Hotline at 1–800–MEDICARE (1–800–633–4227). For the hearing impaired, the telephone number is 1–877–486–2048.
Women who need a diagnostic mammogram should check with their health insurance provider about coverage.
How can uninsured or low-income women obtain a free or low-cost screening mammogram?
Some state and local health programs and employers provide mammograms free or at low cost. For example, the Centers for Disease Control and Prevention (CDC) coordinates the National Breast and Cervical Cancer Early Detection Program. This program provides screening services, including clinical breast exams and mammograms, to low-income, uninsured women throughout the United States and in several U.S. territories. Contact information for local programs is available on the CDC website or by calling 1–800–CDC–INFO (1–800–232–4636).
Information about free or low-cost mammography screening programs is also available from NCI’s Cancer Information Service at 1–800–4–CANCER (1–800–422–6237) and from local hospitals, health departments, women’s centers, or other community groups.
What should women with breast implants do about screening mammograms?
Women with breast implants should continue to have mammograms. (A woman who had an implant following a mastectomy should ask her doctor whether a mammogram of the reconstructed breast is necessary.)
Implants can hide some breast tissue, making it more difficult for the radiologist to detect an abnormality on the mammogram. It is important to let the mammography facility know about breast implants when scheduling a mammogram. The technologist and radiologist must be experienced in performing mammography on women who have breast implants.
If the technologist performing the procedure is aware that a woman has breast implants, steps can be taken to make sure that as much breast tissue as possible can be seen on the mammogram. A special technique called implant displacement views may be used.
What is digital mammography? How is it different from conventional (film) mammography?
In the United States, digital mammography has replaced conventional mammography. Digital and conventional mammography both use x-rays to produce an image of the breast; however, in conventional mammography, the image is stored directly on film, whereas, in digital mammography, an electronic image of the breast is stored as a computer file. This digital information can be enhanced, magnified, or manipulated for further evaluation more easily than information stored on film. Digital images can also be shared electronically, making virtual (remote) consultations between radiologists and breast surgeons easier.
Digital mammography can be done only in facilities that are certified to practice conventional mammography and have received FDA approval to offer digital mammography. The procedure for having a mammogram with a digital system is the same as with conventional mammography.
What is 3-D mammography (also known as tomosynthesis mammography)?
Three-dimensional (3-D) mammography, also known as digital breast tomosynthesis (DBT), is a type of digital mammography in which x-ray machines are used to take pictures of thin "slices" of the breast from different angles and computer software is used to reconstruct an image. This process is similar to how a computed tomography ( CT ) scanner produces images of structures inside of the body. 3-D mammography uses very low dose x-rays, but, because it is generally performed at the same time as standard two-dimensional (2-D) digital mammography, the radiation dose is higher than that of standard mammography. Newer tomosynthesis strategies allow DBT to be done alone, potentially reducing the radiation dose to a level closer to that of standard mammography.
Although many women are offered DBT, it has not yet been determined conclusively whether it is superior to 2-D mammography at identifying early cancers and avoiding false-positive results.
A large-scale randomized breast screening trial is comparing 3-D mammography with 2-D mammography. The Tomosynthesis Mammography Imaging Screening Trial (TMIST) is comparing the number of advanced cancers detected in women screened for 4 years with DBT with that detected in women screened with standard digital mammography.
What other technologies or strategies are being developed for breast cancer screening?
NCI is supporting the development of several new technologies to detect breast tumors. This research ranges from methods being developed in research labs to those that are being studied in clinical trials . Efforts to improve conventional mammography include digital mammography , magnetic resonance imaging (MRI), positron emission tomography (PET) scanning, and diffuse optical tomography, which uses light instead of x-rays to create pictures of the breast.
The Women Informed to Screen Depending on Measures of Risk ( WISDOM ) study is a randomized trial that is testing a personalized approach to breast cancer screening. This 5-year study, which will involve about 100,000 women in California and the Midwest, aims to determine if risk-based screening—that is, screening at intervals that are based on each woman’s risk as determined by her genetic makeup, family history, and other risk factors—is as safe, effective, and accepted as annual screening.
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Mammogram 101: Q&A with a Mammographer
Did you know you don’t need a referral, prescription or order form from your doctor to get a mammogram ? Women over 40 who are not experiencing symptoms can make an appointment for their annual mammogram on their own.
Annual mammograms are the best tool for early detection of breast cancer. Most cancers detected by mammography have no symptoms.
To give you a behind-the-scenes perspective of your annual mammogram, a mammographer from Johns Hopkins Medical Imaging , answers some commonly asked questions about how to prepare for your mammogram, who conducts them, who reads them and what happens after your exam.
What should I do to prepare for my mammogram?
Once you make your appointment for your annual mammogram, you don’t have to do much. Breasts can be tender the week before and during menstruation, so try to schedule your mammogram for one to two weeks after your period starts. We ask women to not wear deodorant, powder, lotion or perfume on the day of their exam as they could show up on the mammogram. For your comfort, we recommend wearing a two-piece outfit, so you are able to keep your pants or skirt on during the mammogram.
If you are breastfeeding or think you may be pregnant, please check with your doctor before scheduling your exam.
Who performs my mammogram?
Mammograms are done by licensed, board-certified technologists called mammographers. Mammographers are specially trained to perform and review breast images of the highest quality with the least amount of radiation exposure. Johns Hopkins mammographers are subspecialized and only conduct breast exams.
We want patients to know that “as a mammographer, I am here to work with you to make this experience as comfortable as possible, to obtain a quality mammogram and ensure your breast health is taken care of.”
Who interprets my mammogram images?
You may never meet your radiologist, but the radiologist is a critical part of your health care team, working with your doctor to keep you healthy or find out why you are sick. Radiologists interpret mammogram and other screening and diagnostic images.
Radiologists are doctors who have continued their education to complete a four-year residency in radiology. A radiologist may act as a consultant to your doctor, or act as primary doctor in treating a disease.
Johns Hopkins breast imaging radiologists are subspecialty radiologists. This means they are fellowship trained, which provides additional training in all aspects of a specific body area or condition, and only read images in that area of expertise. Johns Hopkins breast imaging radiologists only read breast images and are able to focus on the unique aspects of each breast image. Studies have shown that subspecialist radiologists detect more cancers and more early-stage cancers and have lower callback rates than general radiologists.
Karen Horton , director of Johns Hopkins Medicine’s Department of Radiology and Radiological Science , explains the radiologist’s role: “I view myself as a detective trying to diagnose the patient’s problem by combining medical images with other information in the medical record to solve the mystery. Radiology is a unique medical specialty because we use imaging technology to see what is happening on the inside of the body to diagnose and treat disease. We combine high-resolution images with multiple sets of medical record data (patient history, symptoms, demographics, etc.) to determine why a patient is ill to help the referring physician chart the best plan of action to heal the patient.”
What happens after my mammogram?
There is typically no special type of care following a mammogram. However, your health care provider may give you additional instructions depending on your specific health condition.
The radiologist will send the report to your doctor and be a resource in creating an action plan if needed. If you are asked to come back for additional images, don’t be alarmed. In the United States, approximately 5 to 15 percent of women are called back for additional imaging. Additional images might be another mammogram or a different imaging method, such as ultrasound or MRI. The findings of this additional imaging are usually benign, meaning the changes are not caused by cancer.
What happens to the images?
The majority of women will have benign changes in their breasts caused by hormones or the aging process. Through yearly mammograms, these changes can be tracked and monitored. Previous images will be used as a resource to monitor any changes in the breast and flag suspicious changes.
What can I do to be proactive in my breast health if I’m not 40 yet?
Your health care provider should perform a clinical breast exam at your annual physical, and you can practice breast self-awareness by knowing what is normal for your breast and being able to identify small changes immediately. You should perform breast self-exams at least once a month at the same time frame in your menstrual cycle.
Women who are at an increased risk of breast cancer should talk with their health care providers about starting mammography screening earlier than 40, having additional tests (such as breast ultrasound or MRI), or having more frequent exams.
Increased risk can include:
- Family history
- Genetic tendency
- Breast density
- Past breast cancer
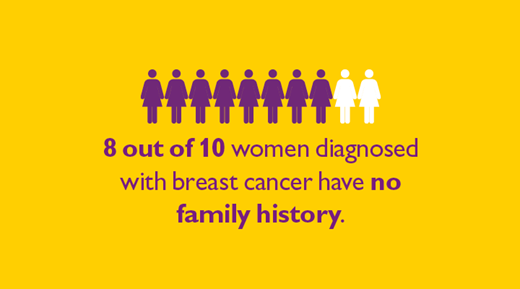
Eight out of 10 women who are diagnosed with breast cancer have no family history; being proactive about your breast exam is a critical step in your overall health.
Schedule Your Mammogram
Find a doctor.
Specializing In:
- Mammography
- Breast Health
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Radiology and Radiological Science
- Breast Imaging
Find Additional Treatment Centers at:
Request an Appointment
Anatomy of the Breasts

Breast Pain 10 Reasons Your Breasts May Hurt

Mammograms and More: Breast Cancer Screening Guidelines
Related Topics
What Is a Mammogram?

Regular mammograms are the best tests doctors have to find breast cancer early.
A mammogram is an X-ray picture of the breast. Doctors use a mammogram to look for early signs of breast cancer. Regular mammograms can find breast cancer early, sometimes up to three years before it can be felt.
How is a mammogram done?
You will stand in front of a special X-ray machine. A technologist will place your breast on a plastic plate. Another plate will firmly press your breast from above. The plates will flatten the breast, holding it still while the X-ray is being taken. You will feel some pressure. The steps are repeated to make a side view of the breast. The other breast will be X-rayed in the same way. You will then wait while the technologist checks the X-rays to make sure the pictures do not need to be redone. Keep in mind that the technologist cannot tell you the results of your mammogram. Each woman’s mammogram may look a little different because all breasts are a little different.
What does having a mammogram feel like?
Having a mammogram is uncomfortable for most women. Some women find it painful. A mammogram takes only a few moments, though, and the discomfort is over soon. What you feel depends on the skill of the technologist, the size of your breasts, and how much they need to be pressed. Your breasts may be more sensitive if you are about to get or have your period. A doctor with special training, called a radiologist, will look at the X-ray for early signs of breast cancer or other problems.
- Try not to have your mammogram the week before you get your period or during your period. Your breasts may be tender or swollen then.
- On the day of your mammogram, don’t wear deodorant, perfume, or powder. These products can show up as white spots on the X-ray.
- Some women prefer to wear a top with a skirt or pants, instead of a dress. You will need to undress from your waist up for the mammogram.
When will I get the results of my mammogram?
You will usually get the results within a few weeks, although it depends on the facility. A radiologist reads your mammogram and then reports the results to you and your doctor. If there is a concern, you will hear from the mammography facility earlier. Contact your health care provider or the mammography facility if you do not receive a report of your results within 30 days.
What happens if my mammogram is normal?
Continue to get mammograms according to recommended time intervals. Mammograms work best when they can be compared with previous ones. This allows the radiologist to compare them to look for changes in your breasts.
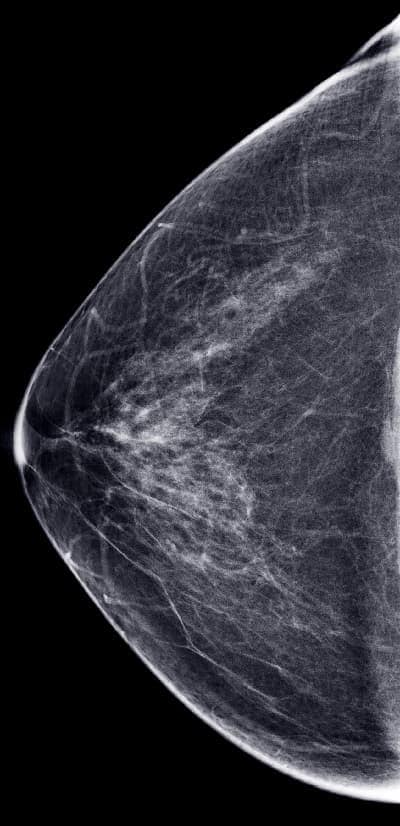
An example of a normal mammogram. Each woman’s mammogram may look a little different because all breasts are a little different.
What happens if my mammogram is abnormal?
An abnormal mammogram does not always mean that there is cancer. But you will need to have additional mammograms, tests, or exams before the doctor can tell for sure. You may also be referred to a breast specialist or a surgeon. It does not necessarily mean you have cancer or need surgery. These doctors are experts in diagnosing breast problems. Doctors will do follow-up tests to diagnose breast cancer or to find that there is no cancer.
Where can I get a mammogram and who can I talk to if I have questions?
- If you have a regular doctor, talk to him or her.
- Contact the National Cancer Institute.
- For Medicare information, you can call 1-800 MEDICARE (1-800-633-4227) or visit The Centers for Medicare & Medicaid Services.
- CDC’s National Breast and Cervical Cancer Early Detection Program works with health departments and other groups to provide low-cost or free mammograms to women who qualify. Find out if you qualify.
Find a mammography facility in your state or territory
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Patient Care & Health Information
- Tests & Procedures
Schedule a screening mammogram
Having a screening mammogram every year is recommended for women over 40. Before you schedule your appointment, consider contacting your insurance provider for information about screening mammogram coverage.
Returning patients
New patients.
Schedule your screening mammogram online.
Online scheduling is available for the following locations:
- Jacksonville
- Cannon Falls
- Chippewa Falls
- Prairie du Chien
For appointments at other locations
Request an appointment online.
Or call Mayo Clinic's Central Appointment Office:
- 507-538-3270
- 7 a.m. to 6 p.m.
- Central time
- Monday through Friday
International patients
International patients can request an appointment at any Mayo Clinic location.
Appointment requests for international patients
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Health Conditions
Get Tested for Breast Cancer

Take Action
Breast cancer is one of the most common kinds of cancer in women. About 1 in 8 women in the United States will get breast cancer during her lifetime.
The good news is that mammograms can help find breast cancer early — before it spreads to other parts of the body. Most women can survive breast cancer if it’s found and treated early.
How often should I get mammograms?
- If you’re age 40 to 49, talk with your doctor about when to start getting mammograms and how often to get them
- If you’re age 50 to 74, get mammograms every 2 years
What is a mammogram?
A mammogram is an x-ray picture of the breast. Mammograms use a very low level of x-rays, which are a type of radiation. The risk of harm from this radiation is very low.
Mammograms can be used to screen (test) for breast cancer in women with no signs or symptoms. They can also help doctors figure out if cancer is causing a particular symptom — like a lump or another change in the breast.
When you get a mammogram, a technician will place your breast on a platform and a plastic plate will press it flat to get a clear picture. This part of a mammogram can be uncomfortable, but it usually only lasts 15 to 20 seconds.
It takes about 20 minutes total to get mammograms. Learn more about mammograms .
Breast Cancer
What is breast cancer.
Breast cancer is cancer that forms in breast tissue. Like all cancers, breast cancer can spread to other parts of the body.
Talk with your doctor or nurse if you notice any of these changes:
- A lump or an area that feels very firm in the breast or armpit
- A change in the size, shape, or feel of the breast
- Fluid (called discharge) coming out of a nipple
- Skin on the breast that is itchy, red, flaky, or dimpled
Learn more about breast cancer .
What if the doctor finds something in my breast?
Mammograms let the doctor or nurse look for lumps or other changes inside your breasts that you can’t feel from the outside. If your doctor finds a lump or another change in your breast tissue, you may need other tests to find out if it’s cancer or not.
The doctor or nurse may take a small bit of tissue from the breast for testing. This procedure is called a biopsy.
See Your Doctor
Talk with your doctor about when and how often to get mammograms.
Ask the doctor about your risk for breast cancer.
Use these questions to start a conversation with your doctor about mammograms . You can also ask about ways you may be able to lower your risk for breast cancer.
Tell your doctor if breast or ovarian cancer runs in your family — that may increase your risk for developing these and other types of cancer. You can use these questions to talk with your doctor about genetic testing for breast or ovarian cancer .
Together, you and your doctor can decide what’s best for you.
Cost and Insurance
What about cost.
Under the Affordable Care Act, insurance plans must cover mammograms for women over age 40. Depending on your insurance plan, you may be able to get mammograms at no cost to you. Check with your insurance company to find out more.
Medicare also covers mammograms for women over age 40 at no cost. Find out about Medicare coverage for mammograms .
If you don’t have insurance, you can still get mammograms. Find a program near you that offers free or low-cost mammograms .
To learn more, check out these resources:
- Free preventive care for women covered by the Affordable Care Act
- How the Affordable Care Act protects you
- Understanding your health insurance and how to use it [PDF - 698 KB]
Healthy Habits
Get support..
Use these tips to get support when you get mammograms.
- Ask other women who have had mammograms about what to expect
- Ask a family member or friend to go with you when you get mammograms
Make sure to ask when you’ll get your mammogram results. When you get the results, ask the doctor or nurse to explain what the results mean. Learn more about mammogram results .
Get active.
Being active increases your chances of living longer. Physical activity helps prevent several types of cancer, including breast cancer. Learn more about how to get active .
Get your well-woman visit.
Get a well-woman visit every year. Use this visit to talk with your doctor or nurse about important screenings and services to help you stay healthy. Learn more about well-woman visits .
Content last updated July 15, 2022
Reviewer Information
This information on breast cancer was adapted from materials from the National Cancer Institute and the Office on Women’s Health.
Reviewed by: Rebecca Chasan, Ph.D. Chief, Science Writing and Review Branch Office of Communications and Public Liaison National Cancer Institute National Institutes of Health
August 2021
You may also be interested in:


Get Screened

Genetic Testing to Learn About Your Risk of Breast and Ovarian Cancer: Questions for the Doctor

Mammograms: Questions for the Doctor
The office of disease prevention and health promotion (odphp) cannot attest to the accuracy of a non-federal website..
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
Your Account
Manage your account, subscriptions and profile.
MyKomen Health
ShareForCures
In Your Community
In Your Community
View resources and events in your local community.
Change your location:

Susan G. Komen®
One moment can change everything.
Breast Cancer Screening for Women at Average Risk
Mammography is the most effective screening tool used today to find breast cancer in most women. However, the benefits of mammography vary by age.
Learn about mammography for women ages:
- 70 and older
Figure 3.1 (below) shows the breast cancer screening recommendations for women at average risk from some major health organizations [ 168-170 ].
Learn about screening recommendations for women at higher risk of breast cancer .
Figure 3.1: Breast cancer screening recommendations for women at average risk
Find questions to ask your health care provider about screening mammography .
Click on the topics below to learn more.
Figure 3.1 shows breast cancer screening recommendations for women at average risk.
Benefits of screening mammography for women ages 40-49
Screening mammography in women ages 40-49 may lower the risk of dying from breast cancer, though the benefit is less than for older women [ 16,34 ].
Komen believes all women should have access to regular screening mammograms when they and their health care providers decide it’s best based on their risk of breast cancer.
The American Cancer Society states women should have the option to have a mammogram every year, starting at age 40 [ 168 ]. It recommends screening mammography every year starting at age 45 [ 168 ].
Risks of screening mammography for women ages 40-49
Overdiagnosis and overtreatment are risks of screening mammography. Overdiagnosis and overtreatment occur when a mammogram finds a cancer that never would have caused symptoms or problems if it had never been diagnosed and had been left untreated.
Another drawback of mammography in women ages 40-49 is a high rate of false positive results (when a screening test shows an abnormal finding that may be cancer when in fact, cancer isn’t present) [ 34-35 ]. Younger women are more likely than older women to have a false positive result on a mammogram [ 35 ].
Getting a false positive result means women will be told they have an abnormal finding and undergo follow-up tests. These tests may include a diagnostic mammogram , breast ultrasound or even a biopsy .
Learn more about follow-up of an abnormal mammogram .
Why are there different screening recommendations for women ages 40-49?
Screening mammography in women ages 40-49 may lower the risk of dying from breast cancer, though the benefit is less than for older women [ 16,34 ]. Some major health organizations have concluded the modest potential benefits of screening mammography for women in their 40s may not outweigh the risks of overdiagnosis, overtreatment and false positive results [ 35 ].
Komen believes all women should have access to regular screening mammograms when they and their health care providers decide it’s best based on their risk of breast cancer.
The American Cancer Society states women ages 40-44 should have the option to have a mammogram every year [ 168 ]. It recommends screening mammography every year starting at age 45 [ 168 ].
The National Comprehensive Cancer Network (NCCN) recommends screening mammography for women every year starting at age 40 [ 169 ].
The U.S. Preventive Services Task Force recommends screening mammography for women every 2 years starting at age 40 [ 170 ].
The American College of Physicians recommends women 40-49 talk with their health care providers about their risk of breast cancer and the pros and cons of screening mammography [ 35 ]. Then, together, they should make informed decisions about when to start getting mammograms and how often to get screened [ 35 ].
Informed decisions are guided by a woman’s breast cancer risk profile. Women at higher risk of breast cancer are more likely to benefit from routine screening mammography than other women [ 35,168-170 ].
Decisions should also be guided by a woman’s preferences based on the potential benefits and risks of mammography [ 35,168-170 ].
Talk with your health care provider about when to start getting mammograms.
Learn more about weighing the benefits and risks of screening mammography , including information on overdiagnosis and overtreatment.
Benefits of screening mammography for women ages 50-69
For women ages 50-69, the benefits of screening mammography are clear. Mammography lowers a woman’s risk of dying from breast cancer. It’s recommended women ages 50-69 have mammograms on a regular basis.
Individual study findings on the benefits of screening mammography vary.
A meta-analysis that combined the results from 6 randomized controlled trials found [ 34 ]:
- Women ages 50-59 who got mammograms on a regular basis had a 14% lower risk of dying from breast cancer than women who didn’t get mammograms.
- Women ages 60-69 who got mammograms on a regular basis had a 33% lower risk of dying from breast cancer than women who didn’t get mammograms.
How often should women ages 50-69 get mammograms?
The American Cancer Society recommends screening mammography every year for women ages 50-54 and every 1-2 years for women ages 55 and older [ 168 ].
The NCCN recommends screening mammography every year for women ages 50-69 [ 169 ].
The U.S. Preventive Services Task Force recommends screening mammography every 2 years for women 50-69 [ 170 ]. The Task Force reviewed the scientific evidence and concluded mammography every 2 years gives almost as much benefit as mammography every year while reducing risks [ 171 ]. These risks include false positive results , overdiagnosis and overtreatment .
If you’re 50-69, talk with your health care provider about how often to get a mammogram.
Figure 3.1 shows breast cancer screening recommendations for women at average risk.
There are few studies (and no randomized controlled trials) on the benefits of screening mammography in women ages 70 and older.
Breast cancer risk increases with age, and mammography doesn’t appear to be less effective in women 70 and older. However, there are risks of mammography in older women, including overdiagnosis and overtreatment.
Many major health organizations, including the American Cancer Society, recommend women ages 70 and older continue to get mammograms on a regular basis as long as they are in good health [ 35-36,168-169 ].
The U.S. Preventive Services Task Force recommends mammography every 2 years for women ages 70-74 [ 170 ]. For women ages 75 and older, the Task Force feels there’s not enough scientific evidence to recommend for or against routine mammography [ 170 ].
Komen believes all women should have access to regular screening mammograms as long as they and their health care providers decide it’s best based on their risk of breast cancer.
Some women may stop routine breast cancer screening due to poor health. Women who have one or more serious health problems may not benefit enough from having breast cancer found early to justify screening.
However, women who are in good health and could benefit from treatment (if breast cancer were found) should continue to get mammograms.
If you aren’t sure whether you should continue getting mammograms, talk with your health care provider.
Although screening mammography saves lives, it has some risks. The benefits and risks of mammography vary by age.
Learn about the benefits and risks of screening mammography .
Updated 05/03/24
TOOLS & RESOURCES
Breast Cancer Screening and Follow-Up Tests

- See All Locations
- Primary Care
- Urgent Care Facilities
- Emergency Rooms
- Surgery Centers
- Medical Offices
- Imaging Facilities
- Browse All Specialties
- Diabetes & Endocrinology
- Digestive & Liver Diseases
- Ear, Nose & Throat
- General Surgery
- Neurology & Neurosurgery
- Obstetrics & Gynecology
- Orthopaedics
- Pain Medicine
- Pediatrics at Guerin Children’s
- Urgent Care
- Medical Records Request
- Insurance & Billing
- Pay Your Bill
- Advanced Healthcare Directive
- Initiate a Request
- Help Paying Your Bill
.cls-1{fill:#2e64ab;}.cls-2{fill:#fff;} CS-Blog Cedars-Sinai Blog
What to expect at your first mammogram.
Oct 18, 2018 Katie Rosenblum

Getting ready for your first mammogram can be a little scary. You might be imagining a machine flattening your breasts like a pancake—and let's face it, that's not a fun visual.
"Everybody knows somebody who's had a mammogram, and there are always horror stories," says Jenny Ton, mammography technologist at Cedars-Sinai . "All you've heard are bad things."
But the truth is, mammograms save lives and are something that should be done annually starting at age 40. The good news is that with a little bit of preparation, the exam can be a lot less stressful.
"Mammography is an early-detection tool, if we do find something, it's usually in the early stages and helps give patients the best outcomes."
What is a mammogram?
A mammogram is a low-dose imaging system used to examine breast tissue. It can help doctors detect abnormalities, like lumps that are too small to be felt, and research has shown that annual mammograms can help detect cancer earlier—when it is most treatable.
"Mammography is an early-detection tool," says Jenny. "If we do find something, it's usually in the early stages and helps give patients the best outcomes."
Read: What’s My Breast Cancer Risk?
What to expect during your mammogram?
When you arrive, you will undress from the waist up and will be given a gown to wear. It's important that you do not wear deodorant, lotions, oils, or perfumes on the day of your exam, as these will interfere with the machine.
During the mammogram, you and a trained technician will be the only ones in the exam room. The tech will position your breasts one at a time in between 2 plastic imaging plates, which will apply pressure while taking the X-ray images. Multiple images will be taken from different positions.
"It can be uncomfortable, but we need to apply the pressure to spread out the tissue so that we get a clearer image of the breast tissue," says Jenny. "The more pressure that is applied, the less radiation will be needed to get an optimal image."
Jenny says this is the most important part, but it's also the part patients dread the most.
"The reaction is usually to tense up, but if you're anticipating pain, you will tense up and your muscle will be fighting the machine," she says. "The more relaxed you are, the easier it is to tolerate."
The entire exam will only take about 10 minutes.
Read: Demystifying Mammograms
"When we're done, patients usually tell me it wasn't nearly as bad as they had been imagining," Jenny says.
If your doctor ordered a diagnostic mammogram due to a change in symptoms, a radiologist will review your scans while you are there. Additional imaging, like an ultrasound, may be requested.
If your doctor ordered a screening mammogram or you needed further imaging, a radiologist will read your scans and send a report to your physician, usually within 48 hours.
It's important to remember that it's not uncommon to get results that indicate suspicious findings. Often, these results are benign and could be caused by dense breast tissue or cysts.
While the thought of getting your first mammogram might seem daunting, it's important to make it a regular part of your preventive healthcare routine.
Ready to schedule your mammogram? Call the S. Mark Taper Foundation Imaging Center at 310-423-8000 for appointments.

Popular Categories
Blog & magazines, popular topics, make an appointment, call us 7 days a week, 6 am - 9 pm pt, support cedars-sinai.
- About Breast Cancer
- Find Support
- Get Involved
- Free Resources
- Mammogram Pledge
- Wall of Support
- In The News
- Recursos en Espa ñ ol
National Mammography Program
- Patient Navigator Program
- Metastatic Retreats
- Support Group
- Breast Health Education
- Breast Cancer Awareness in the Workplace
- Breast Cancer Research
Through our partner facilities, we provide free mammograms and diagnostic services for women in need.
To support our mission, we manage a network of partner medical facilities across the United States. Through this network we provide grants for free breast screening and diagnostic services to those in need (low-income/uninsured/underinsured). These facilities have the systems and partnerships in place to ensure access to treatment for patients who are diagnosed.
The types of services covered include:
- Screening mammograms
- Diagnostic mammograms
- Tomosynthesis (3D mammograms)
- CAD (computer-aided detection)
- Clinical breast exams
- Ultrasounds
- Biopsies (limited)

If there is not an NBCF partner facility in your area, visit our breast cancer resources page for other resources near you. Ask about financial assistance programs, if needed.
NEW! Patient Relief Fund
In collaboration with our hospital partners, NBCF has created the Patient Relief Fund to help ease the cost of breast cancer treatment, making it easier for patients to focus on survivorship.
Help support women in need
Donations are always appreciated, but there are lots of great ways to get involved.
We use cookies on our website to personalize your experience and improve our efforts. By continuing, you agree to the terms of our Privacy & Cookies Policies.
Get screened for breast cancer starting at age 40, new recommendations say
Women should get a mammogram every other year starting at age 40, according to new guidance issued Tuesday by the U.S. Preventive Services Task Force.
It's a considerable drop in age from the prior recommendations, which said women should start getting biennial screenings no later than age 50 and suggested that women in their 40s could talk to their doctor about getting screened.
The change, first released as a draft last year, is a response to rising cancer rates among women in their 40s, as well as evidence that earlier mammograms help save lives. The rate of breast cancer among women ages 40 to 49 increased 2% per year, on average, from 2015 to 2019, according to the National Cancer Institute .
“With this increasing incidence of breast cancer in women in their 40s, that points to mammography being even more beneficial,” said Dr. Wanda Nicholson, the chair of the task force.
The group, an independent panel of experts, estimated that its new recommendations — which were published Tuesday in the journal JAMA — could save up to 20% more lives relative to the old guidance.
Mammograms are essentially X-ray images of the breast. Primary care doctors or obstetrician-gynecologists order them for patients, and the scans are typically done by a technician at an imaging center or radiology department. Patients place each breast between two plates, then a machine images their breast tissue.
If abnormal lesions are found, patients may need additional mammograms, an ultrasound or sometimes a biopsy or MRI to determine if cancer is present.
Insurance companies often follow the task force’s recommendations when determining coverage and reimbursements for preventive screenings; however, most plans already cover mammograms for women starting at age 40, per recommendations from the Health Resources and Services Administration.
The task force's new guidelines do not apply to women with a personal history of breast cancer, those who’ve had an abnormality on a previous biopsy or those with a genetic marker for breast cancer — those groups may need to be screened earlier and more frequently.
The recommendations also only apply to women up to age 74.
Some leading medical groups said the task force's new guidance still does not go far enough.
The American Cancer Society recommends annual screenings — rather than every other year — for women ages 45 to 54, with the option to switch to biennial screenings once they turn 55. It does not recommend that women stop screenings at a certain age, as long as they are expected to live at least 10 more years.
“We are disappointed that the updated USPSTF screening recommendations do not include women over the age of 74,” the ACS said in a statement. “Millions of women over age 75 are in very good health and are expected to live many more years during which their risk of breast cancer remains high.”
But Nicholson said there wasn’t enough evidence for the task force to recommend mammograms to women ages 75 and up.
“We want to reassure people that we have not forgotten women who are 75 years of age and older,” she said. “We are urgently calling for more research for this population.”
The American College of Radiology, meanwhile, expressed disappointment that the task force did not suggest yearly screenings starting at age 40, as the college recommends.
The ACR also suggests that all women — especially Black and Jewish women — talk with their doctors about their breast cancer risk before their 25th birthday. Black women are 40% more likely than white women to die from breast cancer, and Jewish women of Eastern European descent have a higher-than-average risk of breast cancer.
However, the task force's analysis found that getting scans every year can yield more false positive results, which can lead to unnecessary biopsies or women receiving treatment for lesions that don’t necessarily pose a health risk.
“Screening every other year compared to every year had a much more favorable balance of benefits and harms,” Nicholson said.
Dr. Phoebe Freer, chief of breast imaging at the University of Utah’s Huntsman Cancer Institute, said many women would prefer to get screened annually nonetheless.
“Usually, the risk is just being called back for extra pictures — maybe an ultrasound and after that being told that the woman’s fine and she can go back to routine screening. Most women are willing to tolerate that risk for that extra mortality reduction,” she said.
The ACR also recommends an additional MRI each year for women with dense breasts, which is associated with an increased risk of breast cancer . But the task force said it needed more research before suggesting that for women with more dense breast tissue.
"It possible that additional imaging could help them to live healthier, longer lives? The bottom line is that, with our current review, that evidence is just not there," Nicholson said.
Aria Bendix is the breaking health reporter for NBC News Digital.
- Our Story & Mission
- Executive Team
- Patient Stories
- Mona the Mammo Queen
Annual Report
- Audited Financials
Upcoming Events
Hoka hey ride, 35th annual shrimp boil, hats and henna high tea, news & media.

The Rose Named 2024 Non-Profit of the Year by the Pasadena Chamber of Commerce

The Rose Awarded Funds from the Montgomery County Community Foundation

Record-cold temperatures outside, but record-breaking fundraising inside the 3rd Annual Booze and Boobs event benefiting The Rose

My Summer with The Rose

Medicine has never been better. Access to health care has never been worse.

If you are a fan of The Rose and know Dr. Dixie Melillo, this podcast is for you!
- Get Involved
Fundraising
The women of the rose.
- Breast Health/Breast Cancer
- Preparing For Your Visit
- Breast Cancer Support Groups
- Uninsured Patients
- Insured Patients
- Insurance Plans
- Referring Physicians
- Breast Reconstruction Awareness
- Fundraising Opportunities
- The Women of The Rose Book
- Screening/Diagnostics
- Make an Appointment
- 3D Mammography
- Bone Density
- Mobile Mammography Program
- Mammogram to Medical Home Program
- East Texas Hub
- Genetic Testing
- Uninsured Programs
- Solicitud de Cita
- Make Appointment
- News & Media

Phone Alert

Schedule an Appointment

Let's Talk About Your Breasts Podcast

Why Choose The Rose?
We are a breast imaging center of excellence. our mission is saving lives through quality breast health services, advocacy and access to care for all..

Mammogram Screening
An annual mammogram offers peace of mind. Take the time to schedule yours today.

Insured or Uninsured
Regardless of a woman’s ability to pay, we are providing access to screening, diagnostics, and treatment services.

Mobile Mammography
Our 3D Mobile Mammography program services women from Matagorda to Shelby Counties.

3D Technology for all patients
We now offer 3D mammography at our centers and on our mobile coaches.
Making a Difference, Patient by Patient, County by County
Our mission, saving lives through quality breast health services, advocacy and access to care for all., donate today, share your story, schedule your appointment, recent news & blog posts.

United Way of Brazoria County Awards Breast Healthcare Funds

The Rose Welcomes New Board Member Maria Wyckoff Boyce

The Rose raises record $201K for breast cancer care at 34th Annual Shrimp Boil fundraiser

The Rose Recognized by Healthcare Digital Marketing Awards

Quick Links
Terms of use, commitment to privacy, irs form 990, about the rose.
Same day diagnosis, on-site physicians dedicated to breast health care, advanced digital technology—all this reflects The Rose’s emphasis on quality and excellence. The Rose collaborates with the best medical organizations in Texas and reaches women from Matagorda to Shelby Counties.
Latest News
© 2024 The Rose. All rights reserved.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Preventive Care: What's Free and What's Not
Thanks to the Affordable Care Act , health insurers in the U.S. have to cover certain preventive health care without requiring you to pay a deductible , copayment, or coinsurance . That rule applies to all non- grandfathered major medical plans in both the individual/family and employer-sponsored markets.
This article will explain how the preventive care rules work, what services are covered, and what you need to be aware of in terms of potential costs when you go to the doctor for a check-up.
So, what exactly counts as preventive care? Here’s the list of preventive care services for adults that, if recommended for you by your healthcare provider, must be provided free of cost-sharing .
Children have a different list , and there's also an additional list of fully covered preventive services for women .
As long as your health plan isn't grandfathered (or among the types of coverage that aren't regulated by the Affordable Care Act at all, such as short-term health insurance or fixed indemnity plans ), any services on those lists will be fully covered by your plan, regardless of whether you've met your deductible or how long you've been enrolled.
But keep in mind that you'll need to use an in-network medical provider in order to obtain zero-cost preventive care.
Preventive care is one of the ACA's essential health benefits (EHBs). But it's the only one that has to be covered with no cost-sharing . And it's the only one that has to be covered by large group health plans ; the rest of the EHBs only have to be covered on individual/family and small group health plans (although most large employer plans do tend to include all of the EHBs).
Covered preventive care includes:
Cancer prevention measures:
- Colorectal cancer related : for adults age 50 to 75, including screening colonoscopies, removal of polyps discovered during a screening colonoscopy, and anesthesia services required to perform the screening colonoscopy. Note that people do sometimes report being charged for polyp removal during a regular screening colonoscopy, but that is not allowed under federal rules. However, if the colonoscopy is being done in conjunction with any sort of symptoms, or if it's being done more frequently than the normal schedule, it will be considered diagnostic rather than preventive, which means regular cost-sharing rules would apply. For example, if a colonoscopy is being done as a follow-up to a previous colonoscopy in which a polyp was found; doctors sometimes recommend a follow-up after three years, which would generally not be covered by health insurance, since that's outside the regular screening guidelines of once per decade. It's a good idea to thoroughly discuss colonoscopy coverage with your health insurer in order to make sure you fully understand what is and isn't covered under the screening guidelines.
- Breast cancer related : including screening mammograms every 1-2 years for women over 40, BRCA genetic testing and counseling for women at high risk, and breast cancer chemoprevention counseling for women at high risk. As is the case for colonoscopies, mammograms are only covered with zero cost-sharing if they're done purely as a screening measure. If you find a lump in your breast and your healthcare provider wants a mammogram to check it out, your health plan's regular cost-sharing (deductible, copay, and/or coinsurance) will apply, since this will be a diagnostic mammogram rather than a screening mammogram. This will be true even if you've never had a mammogram before, or even if you're due for your regularly-scheduled screening mammogram.
- Cervical cancer related : screening covered once every three years from ages 21 through 65; human papillomavirus DNA testing can instead be done in conjunction with a pap test once every five years.
- Lung cancer related : screening for smokers or those who’ve quit smoking within the last 15 years and are between the ages of 55 and 80
Infectious disease prevention measures:
- Hepatitis C screening one time for anyone born 1945-1965 and for any adult at high risk.
- Hepatitis B screening for pregnant women at their first prenatal visit, and for any adults considered at high risk.
- HIV screening for anyone between ages 15-65, and for others at high risk.
- Syphilis screening for adults at high risk and all pregnant women.
- Chlamydia screening for young women and women at high risk.
- Gonorrhea screening for women at high risk.
- Sexually transmitted infection prevention counseling for adults at increased risk.
- Routine immunizations as recommended by age for
- COVID-19 ( recommendation was added in December 2020 )
- Hepatitis A
- Hepatitis B
- Herpes Zoster(shingles)
- Human Papillomavirus
- Influenza (flu)
- Measles, Mumps, Rubella
- Meningococcal
- Pneumococcal
- Tetanus, Diphtheria, Pertussis (lock-jaw and whooping cough)
- Varicella (chickenpox)
- Obesity screening and counseling.
- Diet counseling for adults at high risk for chronic disease.
- Recommended cardiovascular disease-related preventive measures, including cholesterol screening for high-risk adults and adults of certain ages, blood pressure screening, and aspirin use when prescribed for cardiovascular disease prevention (and/or colorectal cancer prevention) in adults ages 50 to 59.
- Diabetes type 2 screening for overweight adults age 40 to 70
- Abdominal Aortic Aneurysm screening one time for men who have ever smoked
Recommended substance abuse and mental health preventive care:
- Alcohol misuse screening and counseling
- Tobacco use screening and cessation intervention for tobacco users
- Depression screening
- Domestic violence and interpersonal violence screening and counseling for all women
Woman-Specific Preventive Care
- Well-woman visits for women under 65 (note that most Americans transition to Medicare at age 65, and Medicare has its own preventive care coverage).
- Osteoporosis screening for women over 60 based on risk factors.
- Contraception for women with reproductive capacity as prescribed by a healthcare provider. This includes all FDA-approved methods of female contraception, including IUDs, implants, and sterilization. The Supreme Court ruled in 2020 that employers with a "religious or moral objection" to contraception can opt out of providing this coverage as part of their group health plan. But the Biden administration has proposed a rule change that would eliminate the moral objection, and that would ensure access to zero-cost contraception for women whose employers have a religious objection. (Note that although male contraception is not a federally-mandated benefit, some states do require state-regulated health plans to cover vasectomies; state-regulated plans do not include self-insured plans , which account for the majority of employer-sponsored coverage. )
- Preventive services for pregnant or nursing women, including:
- Anemia screening
- Breastfeeding support and counseling including supplies
- Folic acid supplements for pregnant women and those who may become pregnant
- Gestational diabetes screening at 24 and 28 weeks gestation and those at high risk
- Hepatitis B screening at first prenatal visit
- Rh incompatibility screening for all pregnant women and follow up screening if at increased risk
- Expanded tobacco counseling
- Urinary tract or other infection screening
- Syphilis screening
Who Determines Which Preventive Care Benefits Are Covered?
So where did the government come up with the specific list of preventive services that health plans have to cover? The covered preventive care services are things that are:
- Rated “A” or “B” in the current United States Preventive Services Task Force recommendations. (In 2023, a federal judge overturned the requirement that health plans cover preventive services recommended by the USPSTF since 2010. But that ruling has been put on hold while the case is appealed, so health plans must continue to cover these services. )
- Provided for in the comprehensive guidelines supported by the Health Resources and Services Administration (HRSA updated its recommendations for women's preventive services in 2019; the updated guidelines are available here ).
- Recommended by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention
All of the services listed above (and on the lists maintained by HealthCare.gov ) meet at least one of those three guidelines for recommended preventive care. But those guidelines change over time, so the list of covered preventive care services can also change over time. For example, COVID vaccines were added to the list of covered preventive care in December 2020.
If there's a specific preventive care treatment that you don't see on the covered list, it's probably not currently recommended by medical experts. That's the case with PSA screening (it's got a "C" or a "D" rating, depending on age, by USPSTF).
Vitamin D screening is another example of a preventive care service that isn't currently recommended (or required to be covered). For now, the USPSTF has determined that there's insufficient evidence to determine whether to recommend Vitamin D screening in asymptomatic adults. But they do note that more research is needed, so it's possible that the recommendation could change in the future.
It's also important to understand that when you go to your healthcare provider for preventive care, they might provide other services that aren't covered under the free preventive care benefit. For example, if your healthcare provider does a cholesterol test and also a complete blood count, the cholesterol test would be covered but the CBC might not be (it would depend on your health plan's rules, as not all of the tests included in the CBC are required to be covered).
And some care can be preventive or diagnostic, depending on the situation. Preventive mammograms are covered, for example, but your insurer can charge you cost-sharing if you have a diagnostic mammogram performed because you or your health provider find a lump or have a specific concern that the mammogram is intended to address.
Or if you need a follow-up screening sooner than the regular recommended screening guidelines (due to an issue that was found on the last screening test, for example), the follow-up may have your plan's regular cost-sharing. If in doubt, talk with your insurer beforehand so that you'll understand how your preventive care benefits work before the bill arrives.
Preventive Care Related to COVID-19
The COVID-19 pandemic gripped the world starting in early 2020. There's normally a lengthy process (which can last nearly two years) involved with adding covered preventive services through the channels described above.
But Congress quickly took action to ensure that most health insurance plans would fully cover the cost of COVID-19 testing, although that only lasted through the end of the COVID public health emergency, which ended in May 2023.
And the legislation that Congress enacted in the spring of 2020—well before COVID-19 vaccines became available—ensured that once the vaccines did become available, non-grandfathered health plans would cover the vaccine nearly immediately , without any cost-sharing.
ACIP voted in December 2020 to add the COVID-19 vaccine to the list of recommended vaccines, and non-grandfathered health plans were required to add the coverage within 15 business days (well before the vaccine actually became available for most Americans).
That continues to be the case, even after the public health emergency has ended. Recommended COVID vaccines continue to be fully covered by non-grandfathered health plans, just like other recommended vaccines.
Obviously, the medical costs related to COVID-19 go well beyond testing. People who need to be hospitalized for the disease can face thousands of dollars in out-of-pocket costs, depending on how their health insurance plan is structured. Many health insurance companies opted to go beyond the basic requirements, temporarily offering to fully cover COVID-19 treatment , as well as testing, for a limited period of time. But those cost-sharing waivers had mostly expired by the end of 2020.
When Your Health Plan Might Not Cover Preventive Care Without Cost-Sharing
If your health insurance is a grandfathered health plan, it’s allowed to charge cost-sharing for preventive care. Since grandfathered health plans lose their grandfathered status if they make substantial changes to the plan, and can no longer be purchased by individuals or businesses, they’re becoming less and less common as time passes.
But there are still a substantial number of people with grandfathered health coverage; among workers who have employer-sponsored health coverage, 14% were enrolled in grandfathered plans as of 2020. Your health plan literature will tell you if your health plan is grandfathered. Alternatively, you can call the customer service number on your health insurance card or check with your employee benefits department.
If you have a managed care health plan that uses a provider network , your health plan is allowed to charge cost-sharing for preventive care you get from an out-of-network provider. If you don’t want to pay for preventive care, use an in-network provider.
Also, if your health plan is considered an "excepted benefit," it's not regulated by the Affordable Care Act and thus not required to cover preventive care without cost-sharing (or at all). This includes coverage such as short-term health plans , fixed indemnity plans , healthcare sharing ministry plans , and Farm Bureau plans in states where they're exempted from insurance rules.
Preventive Care Isn’t Really Free
Although your health plan must pay for preventive health services without charging you a deductible, copay, or coinsurance, this doesn’t really mean those services are free to you. Your insurer takes the cost of preventive care services into account when it sets premium rates each year.
Although you don’t pay cost-sharing charges when you receive preventive care, the cost of those services is wrapped into the cost of your health insurance. This means, whether or not you choose to get the recommended preventive care, you’re paying for it through the cost of your health insurance premiums anyway.
Under the Affordable Care Act, certain preventive care has to be covered in full (ie, without a deductible, copay, or coinsurance) on all non-grandfathered major medical plans. Covered preventive care includes a long list of services that are recommended by medical experts, although it does not include all medical care that's considered preventive. And some services, such as mammograms, pap test, or colonoscopies—can be fully paid for by the health plan or not. Coverage will depend on whether they're done at regular screening intervals without any symptoms, or to diagnose a problem or follow-up after a previous test returned abnormal results.
A Word From Verywell
Your health plan likely covers a wide range of preventive services at no cost to you, and it's in your best interest to take advantage of these benefits. But to avoid being surprised by an unexpected medical bill, you'll want to be sure you understand the details prior to receiving preventive care. Make sure you use a provider who is in your health plan's network, and make sure you understand exactly what tests or services will be provided during the visit. If you decide to go beyond what your health plan will cover, that's perfectly fine and is a decision you'll make with your medical provider.
U.S. Centers for Medicare & Medicaid Services. Preventive care benefits for adults .
Centers for Medicare and Medicaid Services. Affordable Care Act Implementation FAQs - Set 12 (See Q5) .
Rovner, Julie. Kaiser Health News. High Court Allows Employers To Opt Out of ACA's Mandate On Birth Control Coverage .
U.S. Center for Medicare and Medicaid Services. Coverage of Certain Preventive Services Under the Affordable Care Act: Proposed Rules . January 30, 2023.
Rakoczy, Christy. lendedu. Does Health Insurance Cover the Cost of a Vasectomy?
Kaiser Family Foundation. 2021 Employer Health Benefits Survey .
American Cancer Society. Patient Groups Applaud Circuit Court Ruling That Largely Stays Remedy in Braidwood Management v. Becerra . June 13, 2023.
Health Resources and Services Administration. Women's Preventive Services Guidelines .
Centers for Disease Control and Prevention. Advisory Committee on Immunization Practices (ACIP) .
U.S. Preventive Services Task Force. Final Recommendation Statement: Prostate Cancer: Screening .
U.S. Preventive Services Task Force. Vitamin D Deficiency in Adults: Screening .
Pollitz, Karen. Kaiser Family Foundation. Private Health Coverage of COVID-19: Key Facts and Issues .
America's Health Insurance Plans. Health Insurance Providers Respond to Coronavirus (COVID-19) .
Kaiser Family Foundation. 2020 Employer Health Benefits Survey .
By Elizabeth Davis, RN Elizabeth Davis, RN, is a health insurance expert and patient liaison. She's held board certifications in emergency nursing and infusion nursing.

IMAGES
VIDEO
COMMENTS
A mammogram is an important step in taking care of yourself and your breasts. Whether you're a mammogram newbie or a veteran, knowing what to expect may help the process go more smoothly. How to prepare for your mammogram. If you have a choice, go to a facility that specializes in mammograms and does many mammograms a day.
Women 45 to 54 should get mammograms every year. Women 55 and older can switch to a mammogram every other year, or they can choose to continue yearly mammograms. Screening should continue as long as a woman is in good health and is expected to live at least 10 more years. All women should understand what to expect when getting a mammogram for ...
A mammogram is an x-ray picture of the breast. Mammograms can be used to check for breast cancer in women who have no signs or symptoms of the disease. This type of mammogram is called a screening mammogram. Screening mammograms usually involve two or more x-ray pictures, or images, of each breast. The x-ray images often make it possible to ...
For many women, mammograms are the best way to find breast cancer early, when it is easier to treat and before it is big enough to feel or cause symptoms. Having regular mammograms can lower the risk of dying from breast cancer. At this time, a mammogram is the best way to find breast cancer for most women of screening age. ...
Call the breast center or the hospital's main number. Ask to be transferred to the breast center or women's health center. Once you are transferred, ask who you should speak with about scheduling a free mammogram. If the receptionist doesn't know, ask to speak to a patient or nurse navigator.
443-997-7237 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. A mammographer answers some commonly asked questions about how to prepare for your mammogram, who conducts them, who reads them and what happens after your exam.
Español (Spanish) Print. Regular mammograms are the best tests doctors have to find breast cancer early. A mammogram is an X-ray picture of the breast. Doctors use a mammogram to look for early signs of breast cancer. Regular mammograms can find breast cancer early, sometimes up to three years before it can be felt.
A mammogram is an X-ray image of your breasts. It can be used either for breast cancer screening or for diagnostic purposes, such as to investigate symptoms or unusual findings on another imaging test. During a mammogram, your breasts are compressed between two firm surfaces to spread out the breast tissue.
Follow-up mammograms (diagnostic mammograms) Mammography can be used as a follow-up test when something abnormal is found on a screening mammogram, during a clinical breast exam or when a person notices a change in their breast. A mammogram used as a follow-up test is called a "diagnostic mammogram.". Although it's called a "diagnostic ...
Mammograms are recommended starting at age 40 for women of average breast cancer risk. However, if you have a significant family history of breast cancer, such as one or more first-degree relatives diagnosed with breast cancer, or a first-degree relative diagnosed under the age of 50, then you may need to begin screening earlier.
For appointments at other locations. Request an appointment online. Or call Mayo Clinic's Central Appointment Office: 507-538-3270. 7 a.m. to 6 p.m. Central time. Monday through Friday. PRC-20198295. Patient Care & Health Information.
A mammogram is a low-dose X-ray of breast tissue. Healthcare providers use mammograms, or mammography, to look for early signs of breast cancer before symptoms develop. This is called a screening mammogram. Providers also use mammography to look for any abnormalities if you develop a new symptom, such as a lump, pain, nipple discharge or breast ...
Diagnostic mammogram A diagnostic mammogram is like a screening mammogram, but more images of the breast are taken to examine the abnormal findings more closely. You may get the results from your diagnostic mammogram on the same day. ... To see illustrations of these warnings signs, please visit the breast cancer ...
A mammogram is an x-ray picture of the breast. Mammograms use a very low level of x-rays, which are a type of radiation. The risk of harm from this radiation is very low. Mammograms can be used to screen (test) for breast cancer in women with no signs or symptoms. They can also help doctors figure out if cancer is causing a particular symptom ...
Mammograms. Mammograms are low-dose x-rays that can help find breast cancer. If you've been told you need a mammogram, or you're ready to start breast cancer screening, the topics below can help you know what to expect.
Figure 3.1 shows breast cancer screening recommendations for women at average risk.. Benefits of screening mammography for women ages 40-49. Screening mammography in women ages 40-49 may lower the risk of dying from breast cancer, though the benefit is less than for older women [].Komen believes all women should have access to regular screening mammograms when they and their health care ...
A mammogram is a low-dose imaging system used to examine breast tissue. It can help doctors detect abnormalities, like lumps that are too small to be felt, and research has shown that annual mammograms can help detect cancer earlier—when it is most treatable. "Mammography is an early-detection tool," says Jenny.
They're not for women who have a health condition that may make it hard to diagnose or treat breast cancer. We're here for you. Call us at 1-877-632-6789 or. Breast cancer screening exams help find breast cancer at an early stage. When found early, the chances for successfully treating the disease are greatest.
Screening mammograms are for people without any breast symptoms. You may be eligible to have a screening mammogram even if you have had cancer. Visit Breast Cancer Screening Guidelines to learn about your risk and when to get screened. If you do have symptoms, such as breast lumps or discharge from your breasts, tell your healthcare provider.
National Mammography Program Through our partner facilities, we provide free mammograms and diagnostic services for women in need. ... If there is not an NBCF partner facility in your area, visit our breast cancer resources page for other resources near you. Ask about financial assistance programs, if needed. Search Facilities. NEW! Patient ...
Schedule a Mammogram. Call 206.606.7800 to request a screening mammogram or breast MRI. UW Medicine or Fred Hutch MyChart account users may schedule mammograms online through MyChart. Fred Hutchinson Cancer Center does more than treat breast cancer. We also focus on finding this disease early, when it is easier to treat.
April 30, 2024, 8:00 AM PDT. By Aria Bendix. Women should get a mammogram every other year starting at age 40, according to new guidance issued Tuesday by the U.S. Preventive Services Task Force ...
An annual mammogram offers peace of mind. Take the time to schedule yours today. An annual mammogram offers peace of mind. Take the time to schedule yours today. Search. Search. ... Preparing For Your Visit. Podcast. Breast Cancer Support Groups. Patients. Uninsured Patients. Insured Patients. Insurance Plans. Referring Physicians.
Hepatitis B screening for pregnant women at their first prenatal visit, and for any adults considered at high risk. HIV screening for anyone between ages 15-65, and for others at high risk. ... although it does not include all medical care that's considered preventive. And some services, such as mammograms, pap test, or colonoscopies—can be ...
Regular mammograms to screen for breast cancer should start younger, at age 40, according to an influential U.S. task force. ... Visit focuses on integration of mental health care services in ...