- Skip to primary navigation
- Skip to content

- Billing & Claims Management
- Credentialing & Contracting
- Compliance & Audits
- Revenue Cycle Management
- Primary Care
- Surgical Services
- Midwives and Birth Centers
- Client Stories
- Pay My Bill

Combining a Preventative / Wellness Visit with a Problem-Focused Evaluation / Management Service

As a provider, you have likely found yourself in a scenario wherein you address an issue with your patient during a preventative/wellness visit. Sometimes, you can bill for preventative/wellness and evaluation/management (E/M) visits.
Understanding the nuances of billing in these scenarios helps you bill ethically and legally to receive the maximum compensation for services rendered . The team at Larsen Billing explores combining a preventative/wellness visit with a problem-focused E/M visit below. Read on to learn more.
Combined Billing According to Current Procedural Terminology (CPT®)
It is not uncommon for a patient to present for a preventative/wellness visit, and during the encounter, either the patient may bring up a problem that needs to be addressed, or the provider may identify something abnormal during the visit that warrants a further workup, thereby requiring care that goes beyond the preventative/wellness service.
The provider can often bill for preventative/wellness and problem visits (E/M) when this occurs.
According to the CPT® codebook created and maintained by the AMA :
If an abnormality is encountered or a pre-existing problem is addressed in the process of performing this preventive medicine evaluation and management service, and if the problem or abnormality is significant enough to require additional work to perform the key components of a problem-oriented E/M service, then the appropriate Office/Outpatient code 99201-99215 should also be reported.
CPT® does go on to clarify that “an insignificant or trivial problem/abnormality” identified during the visit but does not require additional workup should not be separately reported.
Modifier 25 should be appended to the office/outpatient code to bill for both services within the same encounter appropriately. Modifier 25 indicates that a significant, separately identifiable evaluation and management service was provided on the same day as the preventative/wellness service.
Providers should meticulously document their charts to distinguish between the two services. It’s best practice for the provider to create two separate encounter notes to identify the preventative/wellness and problem-focused visit.
Determining the Appropriate Level of Service for the Problem-Visit E/M
The level of service for the problem-visit E/M may be based on time or medical decision-making (MDM). We review both levels below.
Level of Service Based on Time
For cases in which a problem visit is being reported during the same encounter as the preventative/wellness visit, coding based on time may be slightly more complicated; the provider must ensure they are only considering the time spent addressing the problem and not time spent on the preventative/wellness service.
For coding purposes, time is the total time that includes both face-to-face time and non-face-to-face time on the day of the encounter.
Included in Total Time
The following elements should be included in the total time:
- Preparing to see the patient (e.g., reviewing external test results)
- Obtaining and/or reviewing separately obtained history
- Performing a medically appropriate examination and/or evaluation
- Counseling and educating the patient, family, or caregiver
- Ordering medications, tests, or procedures
- Referring and communicating with other health care professionals (when not separately reported)
- Documenting clinical information in the electronic or other health records
- Independently interpreting results (not separately reported with a CPT® code) and communicating results to the patient, family, or caregiver
- Care coordination (not separately reported with a CPT® code)
Not Included in Total Time
These elements are not included in the total time:
- Performance of other services that are reported separately
- Teaching that is general and not limited to the discussion that is required for the management of a specific patient
You can find time codes for both new and established patients in the charts below:
Prolonged Visit Codes
When the total time on the date of service extends beyond the times listed above for codes 99205 and 99215 by at least 15 minutes, a prolonged service code may be added, and it can be billed in 15-minute increments.
Level of Service Based on Medical Decision-Making (MDM)
The three elements of MDM include:
- The number and complexity of problems addressed during the encounter
- Data would include information that must be reviewed, obtained, ordered, and analyzed for the encounter
- The risk of complications and/or morbidity or mortality of the patient management
The levels of MDM are categorized into four types:
- Straightforward
- Low complexity
- Moderate complexity
- High complexity
The chart below delineates the level of service based on MDM:
Two out of three elements from the table must be met or exceeded to determine a level of service for an encounter.
For example, a provider may address multiple problems during a visit; however, there is limited data, and the risk is low. In this scenario, the medical decision-making level would qualify as low.
The following table below breaks down the number and complexity of problems addressed:
Preventative Service Codes
Preventative medicine services have unique codes based on the patient’s age and status as either new or established. We include these codes in the chart below:
Preventative Medicine Services
Additionally, Medicare employs a unique code set for preventative services. When billing Medicare for preventative care, enter the appropriate codes found below:
Preventative Services for Medicare
Billing Made Simple
Accurate coding and billing are essential for your practice to receive appropriate payments based on services rendered. Understanding when and how to combine a preventative/wellness visit with a problem-focused E/M visit ensures you optimize your time and talents to receive the highest payment possible.
However, we at Larsen Billing know the time and energy commitment required to execute accurate medical billing and coding practices. If you’re busy caring for patients, neither you nor your team have the time or resources to spend countless hours on coding, billing, and claims manage ent. That’s why we are here.
Larsen Billing provides medical billing and coding services that keep your practice running, ensuring on-time and accurate submissions that reduce claims denials and the highest payment possible. Our team of experts studies coding and regulation updates to keep your practice compliant with every claim submission.
Learn how Larsen Billing can help you focus on patient care while we handle your billing, claims, and compliance n eds. Our team cares about your success and works to that end every step of the way.
Adding {{itemName}} to cart
Added {{itemName}} to cart
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- E/M Coding and Billing Res...
- Office/Outpatient E/M Visi...
- History and Examination
History and Physical Examination
Documenting h&p for office/outpatient e/m services.
Only a "medically appropriate history and/or examination" is required for all office/outpatient E/M codes. The number of body systems/areas reviewed and examined need only be performed and documented when medically necessary and clinically appropriate. This element of reporting was revised by CMS for Medicare patients in an effort to reduce documentation burden.
Additionally, for Medicare patients, billing practitioners do NOT need to re-enter information about a patient's chief complaint and history in the medical record that has already been entered by ancillary staff or the beneficiary. The billing practitioner may simply indicate in the medical record that such information was reviewed and verified. Note that this policy may be different for non-Medicare private payors.
The tables below compare required H&P elements in the current and new CPT code set for the office/outpatient E/M codes.
*Code 99201 was deleted in 2021 and is not included in this table.
**Codes 99211, 99417, and G2212 are not included in this table because H&P elements do not apply when reporting using total time to select a code.
Download the Office E/MT Coding Changes Guide (PDF)

- Become a Member
- Everyday Coding Q&A
- Can I get paid
- Coding Guides
- Quick Reference Sheets
- E/M Services
- How Physician Services Are Paid
- Prevention & Screening
- Care Management & Remote Monitoring
- Surgery, Modifiers & Global
- Diagnosis Coding
- New & Newsworthy
- Practice Management
- E/M Rules Archive
May 8, 2024
Reporting a Problem-Oriented Visit on the Same Day as Welcome to Medicare (G0402) or Initial and Subsequent Wellness Visit (G0438, G0439)
- I continue to hear that some consultants and coders don’t agree with reporting a problem oriented visit with welcome to Medicare or wellness visit
- The 2024 Physician Fee Schedule Final Rule commented on this
What does CMS say about adding an E/M service to a Welcome to Medicare visit or annual wellness visit?
About the Welcome to Medicare visit
When you furnish a significant, separately identifiable, medically necessary Evaluation and Management (E/M) service along with the IPPE, Medicare may pay for the additional service. Report the additional Current Procedural Terminology (CPT) code (99201–99215) with modifier -25. That portion of the visit must be medically necessary to treat the beneficiary’s illness or injury, or to improve the functioning of a malformed body member. [1]
About the Annual Wellness Visit
When you furnish a significant, separately identifiable, medically necessary Evaluation and Management (E/M) service along with the AWV, Medicare may pay for the additional service. Report the additional Current Procedural Terminology (CPT) code with modifier -25. That portion of the visit must be medically necessary to treat the beneficiary’s illness or injury, or to improve the functioning of a malformed body member. [2]
From the 2024 Physician Fee Schedule Final Rule
And, in the 2024 Physician Fee Schedule Rule, in a discussion of initiating visits for Community Health Integration CMS says, “Further, we believe that practitioners would normally bill an E/M visit in addition to the AWV when medical problems are addressed in the course of an AWV encounter, in accordance with our manual policy providing that a medically necessary E/M visit may be billed when furnished on the same occasion as an AWV in those circumstances (Chapter 12, Section 30.6.1.1.H of the Medicare Claims Processing Manual (Pub, 100-04).” [3]
And, “We continue to believe that when an AWV involves diagnosis or treatment of injury or illness to the degree that would warrant subsequent furnishing and billing of CHI to remove barriers significantly limiting the treatment plan, in most cases, an E/M visit would be separately billed.” [4]
CMS appears to be saying that when a Medicare beneficiary requires diagnosis or treatment of an illness, they expect a separate E/M service to be reported.
[1] ABCs of the Initial Preventive Physical Exam (IPPE) , ICN 006904 April 2017 p. 5
[2] ABCs of the Annual Wellness Visit, ICN 905706 April 2017 p. 10
[3] CMS 2024 Physician Fee Schedule Final Rule, p. 309
[4] CMS 2024 Physician Fee Schedule Final Rule, p. 313
If you’ve read anything I’ve written on this topic or watched my videos , you know my opinion:
If the physician/NP/PA treats and documents and manages an acute or chronic problem during the same encounter as a wellness visit, bill both a Welcome to Medicare or Wellness Visit on the same day (hereafter referred to in shorthand as “wellness visits”). Reviewing significant, stable chronic problems counts. The note should show that the condition was reviewed and assessed, especially if there is no change in treatment. I do add a caveat: if the information about the chronic conditions is imported/copied from a prior note with barely an update , then don’t bill for the problem-oriented visit.
One MAC’s Q&A
Q: When a patient is scheduled for a follow up visit of several chronic conditions, is it allowed for the provider to separately bill Annual Wellness Visit performed on the same day? Answer: Some chronic, stable conditions may not require assessment beyond the AWV, while others may require additional clinical examination and review or changes to the plan of care. This decision is within the realm of the performing provider’s clinical judgement. When additional history, examination and MDM is indicated to fully assess a patient’s clinical status, a separate E/M service may be performed and billed. Documentation of the E/M visit should clearly support the medical necessity of the separate service. Added 2/20/2020 Q: When is an E/M service separately payable on the same DOS as the AWV? Answer: The AWV has been designed as an annual overview of the patient’s health status, including elements of physical and mental health and general safety. It may be performed by clinical staff under physician or NPP supervision, and includes a review of known chronic conditions. In some situations, the patient’s chronic (or acute) condition(s) may require evaluation and management by the primary health care provider (physician or NPP). Documentation for these services may be included in one note or in two separate notes, based on the provider’s preference. Of note, the documentation must clearly delineate all necessary details of the AWV and all necessary elements of the E/M service relative to medical necessity and level of coding. Updated 2/20/2020
This NGS answer in a nutshell: sometimes yes, sometimes no.
If one of the patient’s conditions is not stable (as noted in the HPI, exam, assessment and treatment plan) , or, an acute problem is addressed, then do add a problem-oriented visit at the time of the wellness visit. Document the symptoms or the status of the condition in the HPI. If the HPI does not describe the conditions, don’t bill an E/M. The treatment plan should show either a change in treatment or a plan to monitor the condition.
Keep in mind the revised E/M guidelines for codes 99202–99215. Code selection for these office and other outpatient visits is based on time or medical decision making. History and exam are no longer key components in code selection. That makes it easier to meet the code requirements for a problem oriented visit. In my opinion, it is more defensible if the history describes either HPI symptoms for an acute problem or the status of chronic conditions.
And once again, if it is all copied from a prior note, don’t bill it!
Get Unlimited Access to CodingIntel’s Online Library!
Request more information on a CodingIntel membership and see how it can help your practice.
Become a member!
Last revised April 9, 2024 - Betsy Nicoletti Tags: Preventive and problem visits , primary care_preventive services
CPT®️️ is a registered trademark of the American Medical Association. Copyright American Medical Association. All rights reserved.
All content on CodingIntel is copyright protected. Any resource shared within the permissions granted here may not be altered in any way, and should retain all copyright information and logos.
- What is CodingIntel
- Terms of Use
- Privacy Policy
Our mission is to provide up-to-date, simplified, citation driven resources that empower our members to gain confidence and authority in their coding role.
In 1988, CodingIntel.com founder Betsy Nicoletti started a Medical Services Organization for a rural hospital, supporting physician practice. She has been a self-employed consultant since 1998. She estimates that in the last 20 years her audience members number over 28,400 at in person events and webinars. She has had 2,500 meetings with clinical providers and reviewed over 43,000 medical notes. She knows what questions need answers and developed this resource to answer those questions.
Copyright © 2024, CodingIntel A division of Medical Practice Consulting, LLC Privacy Policy

Even an old patient can be new .
EMILY HILL, PA-C
Fam Pract Manag. 2003;10(8):33-36
This is a corrected version of the article that appeared in print.
New patient visits used to be easy to distinguish from those with established patients. A new patient was someone you had not previously seen or perhaps someone for whom you did not have a current medical record. Today, like so many other aspects of health care delivery, differentiating between new and established patients and coding your services accordingly has become more complex.
By CPT definition, a new patient is “one who has not received any professional services from the physician, or another physician of the same specialty who belongs to the same group practice, within the past three years.” By contrast, an established patient has received professional services from the physician or another physician in the same group and the same specialty within the prior three years.
New patient visits require more work than established patient visits at the same level, and this is reflected in the coding requirements as well as the reimbursement for new patient visits.
A key to differentiating between new and established patients is understanding two terms used in CPT’s definition of a new patient: “professional services” and “group practice.”
Medicare’s definition of a new patient is slightly different than CPT’s.
The distinction between new and established patients applies only to the categories of evaluation and management (E/M) services titled “Office or Other Outpatient Services” and “Preventive Medicine Services,” but as a family physician, most of the codes you submit fall into these categories, and the definition is hard to incorporate into your coding habits. This article will explain why the difference matters and describe an approach you can use to make the definition easier to apply.

The key differences
The reason for learning to distinguish new patients from established patients, apart from following coding guidelines, is that it enables you to be reimbursed for the additional work that new patient visits require (see “Documentation requirements” ).
DOCUMENTATION REQUIREMENTS FOR NEW- AND ESTABLISHED-PATIENT OFFICE VISITS
Source: Medicare resource-based relative value scale (RBRVS).
Another important difference between the codes is that the new patient codes (99201–99205) require that all three key components (history, exam and medical decision making) be satisfied, while the established patient codes (99211–99215) require that only two of the three key components be satisfied. Because the criteria for coding problem-oriented new patient visits are more stringent, there are also cases where the same service components would yield an established patient code with more RVUs than the appropriate new patient code. For example, a visit that includes an expanded problem-focused history, detailed problem-focused exam and moderate complexity decision making would qualify as a level-II new patient visit (1.70 RVUs) but a level-IV established patient visit (2.17 RVUs).
Problem-oriented encounters for both new and established patients can also be coded based on the total time spent with the patient if counseling/coordination of care constitutes more than 50 percent of the total encounter time. The times associated with the new patient services, however, are higher than for the established patient encounters. (See “Time Is of the Essence: Coding on the Basis of Time for Physician Services,” FPM, June 2003, page 27 .)
Defining “professional services”
Varying interpretations of what constitutes a “professional service” have been a source of confusion for practices trying to determine which patients qualify as new. CPT 2001 clarified the matter by defining professional services as “those face-to-face services rendered by a physician and reported by a specific CPT code(s).” The key phrases are “face-to-face” and “reported by a specific CPT code(s).”
Suppose you provided the interpretation of an ECG for an inpatient you did not actually meet in person. When you see the patient in your office (assuming this occurs within the next three years), you would report the E/M service you provide using a new patient code since there was no face-to-face encounter during the inpatient stay.
Consider the patient who is new to the community and needs a refill of her oral contraceptives. You agree to call in a prescription that will meet her needs until she can be seen in your office the following week. When you see her for her well-woman visit, you report a new patient preventive medicine service code since you did not have a face-to-face encounter with the patient when calling in her prescription.
If you are in solo practice, all you need to remember to differentiate new patients from established ones is whether you provided a face-to-face service within the last three years. The situation is different, however, for group practices.
Defining “group practice”
Although groups with multiple practice sites may operate independently, with each caring for its own patient population and maintaining its own medical records, they are considered a single group if they have the same tax identification number.
In a single-specialty practice, the patient’s encounter should be reported with a code in a new patient category only if no physician or other provider who reports services using CPT codes in that group has seen the patient within the last three years. For example, let’s say your partner saw a patient who is new to your practice in the emergency department (ED) over the weekend. The following week you see the patient in the office. Since someone else in your practice has seen the patient within the last three years, you have to use an established patient code. This is the case even though the patient had not been seen in the office and there was not an established medical record there.
In a multispecialty practice, a patient might be considered new even if he or she has received care from several other physicians in the group and a medical record is available. The distinguishing factor here is the specialty designation of the provider. For example, take a patient who has been seen regularly by the pediatrician in your group. The patient is now 18 years old and wants to transfer care to a family physician in the same group. When she sees the family physician, she’ll qualify as a new patient because the family physician is in a different specialty than her previous physician. This is the case even though the family physician might be treating her for an existing problem and referring to her established medical record.
Medicare has a list of specialty and sub-specialty designations it recognizes for payment purposes. Other payers may use this same list or may recognize more areas of expertise based on credentialing information.
When you change practices
Consider this scenario: Suppose you leave the practice where you have been working for a number of years to join a new group in a nearby community. Some of your patients transfer their care to the new practice and see you within three years of their last visits. You would report these encounters using an established patient code because, although you are practicing in a new group, you have provided professional services to the patient during the last three years. Note that whether the patient has transferred his or her medical records to your office and how long you may have had those records is irrelevant. The amount of time that’s passed since your last encounter with the patient is the determining factor.
Visits with patients who do not transfer care and are seen by another family physician in the original group within the three-year time frame are reported as established patient encounters. In this instance, the patient’s status is determined by the group identification, the time frame since the last encounter and the specialty of the physician providing care.
When one group provides coverage for another physician group, the patient encounter is classified as it would have been by the physician who is not available. For example, let’s say your practice provides coverage for a solo physician in your community. While the physician is out of town, you see one of her patients. As long as the physician who is out of town has seen the patient in the last three years, you have to report the service using an established patient code. This is true even if you are unfamiliar with the patient, clinical information is not available and the office staff does not have basic demographic information.
Special considerations for Medicare patients
A slightly different approach may be taken when Medicare patients are involved. Medicare has stated that a patient is a new patient if no face-to-face service was reported in the last three years. The group practice and specialty distinctions still apply, but “professional service” is limited to face-to-face encounters. Therefore, if you see a Medicare patient whom you have seen within the last three years, you must report the service using an established patient code. On the other hand, if a lab interpretation is billed but no face-to-face encounter took place, the new patient designation might be appropriate.
Consultations vs. new patient visits
If a patient is sent to you for an opinion or advice, the encounter may be a consultation service rather than a new patient encounter. CPT defines a consultation as “a type of service provided by a physician whose opinion or advice regarding evaluation and/or management of a specific problem is requested by another physician or other appropriate source.” For example, if you are asked to see a patient for a pre-operative clearance or for evaluation of a medical problem, the appropriate category might be consultation services. Since the same consultation codes apply to both new and established patients, it is not necessary to apply the new patient definition.
Decision tree for determining if a patient is new or established
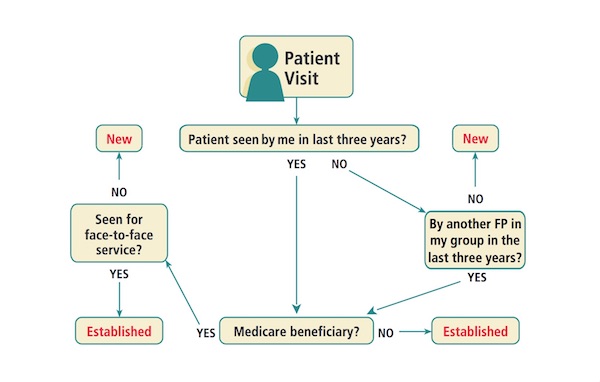
Getting it right
The decision tree will prompt you to ask yourself a series of questions that will help you determine whether to code a new or established patient visit.
Getting it right can help ensure that you get paid appropriately for your services and keep your practice audit-proof.
Continue Reading
More in fpm, more in pubmed.
Copyright © 2003 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

COMMENTS
2021 E/M Office/Outpatient Visit CPT Codes. Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components: A problem focused history; A problem focused examination; Straightforward medical decision making. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided ...
When that service is medically necessary during a Medicare wellness visit, the physician can also bill for a problem-oriented E/M office visit on the same day, again using the appropriate CPT code ...
performing a preventive/wellness visit, and the problem or abnormal finding is significant enough to require additional work to perform the key components of a problem-focused evaluation and management service, then the appropriate office/outpatient E/M code should also be billed. Modifier-25 should be added to the office/outpatient
Problems are the coding key. Code the visit by just looking at your assessment and plan. Quiz. If you're coding outpatient office visits based on medical decision making rather than time, the ...
Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if it does not, go to ...
The codes apply to services that a wide range of primary care and specialty providers perform regularly. Some of the most commonly reported E/M codes are 99201-99215, which represent office or other outpatient visits. In 2020, the E/M codes for office and outpatient visits include patient history, clinical examination, and medical decision ...
If an abnormality is encountered or a pre-existing problem is addressed in the process of performing this preventive medicine evaluation and management service, and if the problem or abnormality is significant enough to require additional work to perform the key components of a problem-oriented E/M service, then the appropriate Office ...
CPT® code 99417 is used to report additional time beyond the time periods required for office/outpatient E/M visits. Additional time includes face-to-face and non-face-to-face activities. Code 99417 may only be used when total time has been used to select the appropriate E/M visit and the highest E/M level has been achieved (i.e., 99205 or 99215).
Same-day Preventive and E/M Services. Sometimes, at a scheduled preventive visit, the patient mentions a new or worsened condition. If the patient complaint requires additional workup, beyond that usually associated with the preventive service, you may choose to report a problem-focused visit in addition to the preventive service.
Summary of Major E/M Revisions for 2021: Office or Other Outpatient Services. •Extensive E/M guideline additions, revisions, and restructuring •Deletion of code 99201 and revision of codes 99202-99215. o Codes 99201 and 99202 currently both require straightforward MDM. •Components for code selection:
Here are five tips to make your claim stronger: Append the modifier 25 on the problem-oriented office visit. Do not count elements related to preventive care toward the problem-oriented level of service. Ensure the ICD-10 code you assign supports the medical necessity for the services. Document the preventive care and the office visit ...
About CPT Code 99213: Office or Other Outpatient Visit for the Evaluation and Management of an Established Patient, Level 3 ... Expanded problem-focused examination. Conduct a thorough physical examination focused on the identified problems. ... CPT Code: Description: Visit Length: 99211: New patient office visit, level 1: 10-19 minutes:
The American Medical Association (AMA) has established new coding and documentation guidelines for office visit/outpatient evaluation and management (E/M) services, effective Jan. 1, 2021. The ...
New Patient Office Visit (E/M) Services (CPT® 99201-99205) — Documentation Requirements. CPT® Code. Description. Documentation Requirements . 99201. Typically 10 minutes . Problem-focused history; Problem-focused exam; Straightforward medical decision-making (Based on straightforward medical decision-making)
The tables below compare required H&P elements in the current and new CPT code set for the office/outpatient E/M codes. New Patient Codes. CPT Code. H&P Elements Prior to 2021. H&P Elements Effective in 2021. 99202. ... Expanded problem focused history/examination. Medically appropriate history and/or examination for all codes. 99214.
The E/M codes for home care services now include any patient residence, including assisted living facilities, which prior to 2023 had a separate code category (99324-99328, 99334-99337). Now all home or residence services are reported using codes 99341-99345 for new patients and 99347-99350 for established patients.
Keep in mind the revised E/M guidelines for codes 99202-99215. Code selection for these office and other outpatient visits is based on time or medical decision making. History and exam are no longer key components in code selection. That makes it easier to meet the code requirements for a problem oriented visit.
CPT® code 99203: New patient office or other outpatient visit, 30-44 minutes. As the authority on the CPT® code set, the AMA is providing the top-searched codes to help remove obstacles and burdens that interfere with patient care. These codes, among the rest of the CPT code set, are clinically valid and updated on a regular basis to ...
For example, a visit that includes an expanded problem-focused history, detailed problem-focused exam and moderate complexity decision making would qualify as a level-II new patient visit (1.70 ...
When reporting the preventive visit (well visit) and a problem-focused visit (sick visit) on the same day, you must append modifier 25 Significant, Tweet. ... Therefore, CPT code 99395 ... Modifier -25 would then be appended to the office visit level of service reported, to indicate that a significant, separately identifiable E/M service was ...
About CPT Code 99201: New Patient Office or Other Outpatient Services, Problem Focused, Minimal Severity. CPT code 99201 pertains to an office or other outpatient visit for the evaluation and management (E/M) of a new patient, categorized as Level 1. This code involves a patient encounter with minimal complexity and includes the following key ...
CPT® code 99213: Established patient office or other outpatient visit, 20-29 minutes. As the authority on the CPT® code set, the AMA is providing the top-searched codes to help remove obstacles and burdens that interfere with patient care. These codes, among the rest of the CPT code set, are clinically valid and updated on a regular basis to ...